In 2011, psychiatrist Lisa Pan described a stunning case study. They were trying to treat a 19-year-old patient suffering from suicidal ideation. Nothing seemed to help. The patient had several suicide attempts; the antidepressants weren’t working. It was a severe situation with no clear fix in sight.
The breakthrough came when researchers realized the patient had a metabolic imbalance. They treated this imbalance and lo and behold — the patient’s depression started going away. Mental function improved significantly, and the suicide ideation pretty much disappeared.
Fast forward a few years and a follow-up study confirmed that a large number of patients with suicide ideation seem to have a detectable metabolic condition that can be addressed.
Now, Pan and colleagues have taken things one step further: they’ve shown a connection between cellular metabolism and depression. Essentially, they found that many people with depression and suicidal ideation had detectable compounds in their blood that could help identify individuals at higher risk of becoming suicidal.
Depression and suicidal thoughts are on the rise
It’s estimated that around 5% of adults worldwide suffer from depression. Major depressive disorder (MDD) has been ranked as the third cause of the burden of disease worldwide in 2008 by the World Health Organization. In addition to causing immense suffering around the world, depression costs $210 billion annually.
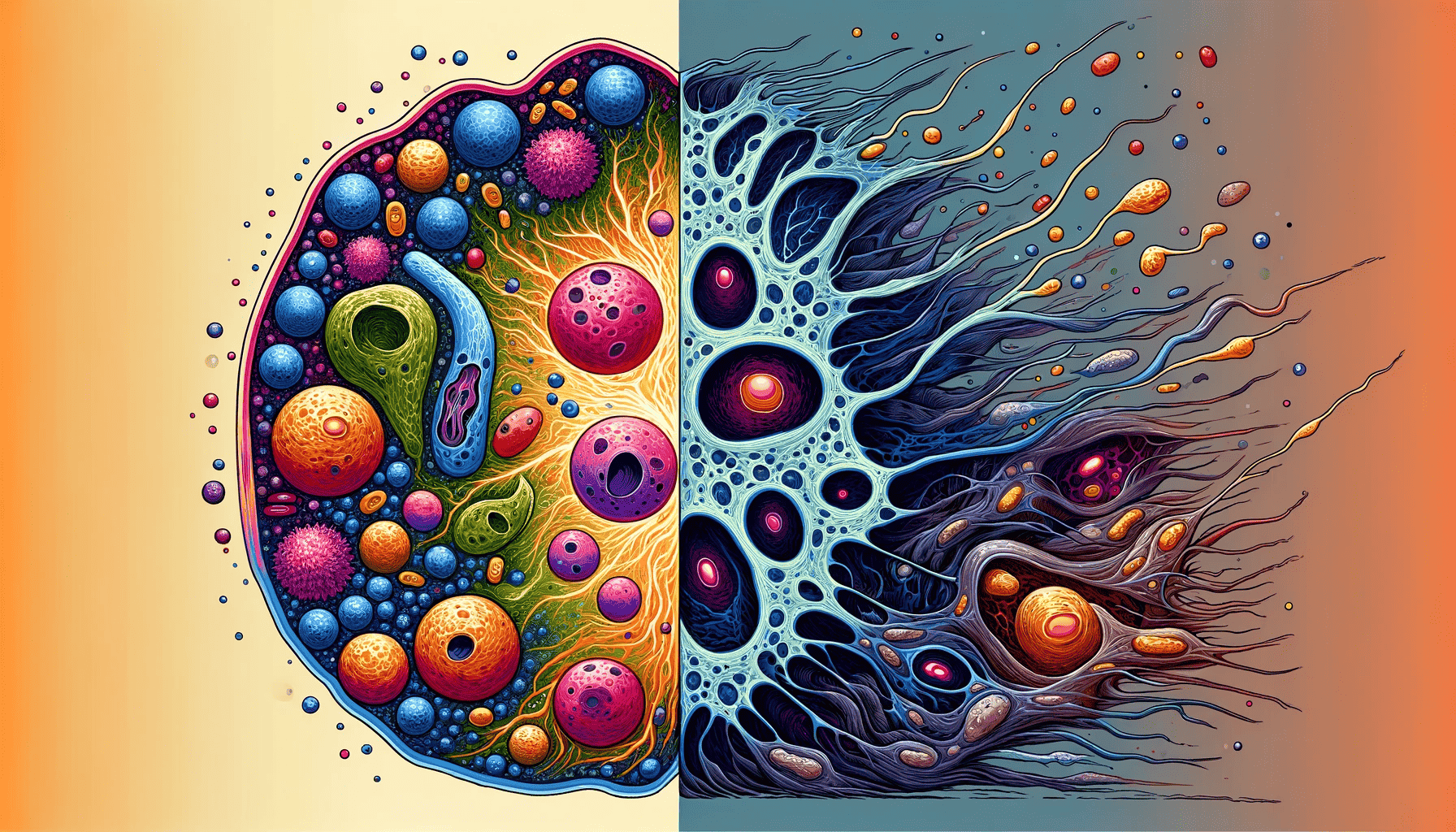
The primary symptoms of depression are psychological, but increasingly, doctors and scientists are showing that depression has tangible physical effects as well. For example, several markers of cellular metabolism appear to be linked with depression, and modern technology is enabling researchers to detect such markers.
“Mental illnesses like depression have impacts and drivers well beyond the brain,” said Robert Naviaux, a study author and professor in the Department of Medicine, Pediatrics and Pathology at UC San Diego School of Medicine. “Prior to about ten years ago it was difficult to study how the chemistry of the whole body influences our behavior and state of mind, but modern technologies like metabolomics are helping us listen in on cells’ conversations in their native tongue, which is biochemistry.”
This approach is especially useful in so-called “treatment-refractory” depression cases — when treatments have little impact. In particular, researchers focused on cases of depression linked with suicidal thoughts.
Suicidal thoughts are common in most treatment-refractory depression cases, and around 1 in 3 out of these cases will attempt suicide at least once.
“We’re seeing a significant rise in midlife mortality in the United States, and increased suicide incidence is one of many things driving that trend,” said Naviaux. “Tools that could help us stratify people based on their risk of becoming suicidal could help us save lives.”
A physical component of suicidal thoughts
Pan, Naviaux, and colleagues analyzed the blood of 99 participants with treatment-refractory depression and suicide ideation. They also included a control group of 99 healthy participants. They tracked hundreds of different biochemicals in their blood and uncovered five of them that can be used as a biomarker to detect treatment-refractory depression and suicide ideation.
This is important not just as a diagnosing mechanism, but also for uncovering the underpinnings of depression, researchers say.
“If we have 100 people who either don’t have depression or who have depression and suicidal ideation, we would be able to correctly identify 85-90 of those at greatest risk based on five metabolites in males and another 5 metabolites in females,” said Naviaux. “This could be important in terms of diagnostics, but it also opens up a broader conversation in the field about what’s actually leading to these metabolic changes.”
Some of these biochemicals are linked to mitochondria. As we’re taught in school, the mitochondria are the powerhouse of the cell — they produce ATP, the primary energy that our cells use. ATP is also important for cell-to-cell communication. However, in cases of suicide ideation, this ATP is dysregulated.
“When ATP is inside the cell it acts like an energy source, but outside the cell it is a danger signal that activates dozens of protective pathways in response to some environmental stressor,” said Naviaux.
“We hypothesize that suicide attempts may actually be part of a larger physiological impulse to stop a stress response that has become unbearable at the cellular level.”
Not a silver bullet
This opens up important avenues for treatment. Some of the metabolic deficiencies identified here are in compounds that are already available as supplements (such as folate or carnitine). Addressing these imbalances could also have a positive effect on depression and suicidal thoughts.
However, researchers stress this is not a magic cure.
“None of these metabolites are a magic bullet that will completely reverse somebody’s depression,” said Naviaux. “However, our results tell us that there may be things we can do to nudge the metabolism in the right direction to help patients respond better to treatment, and in the context of suicide, this could be just enough to prevent people from crossing that threshold.”
Nevertheless, this research suggests an important personalized approach — and not just for depression, but potentially for other conditions at the time.
“Many chronic diseases are comorbid with depression, because it can be extremely stressful to deal with an illness for years at a time,” said Naviaux. “If we can find ways to treat depression and suicidal ideation on a metabolic level, we may also help improve outcomes for the many diseases that lead to depression. Many chronic illnesses, such as post-traumatic stress disorder and chronic fatigue syndrome, are not lethal themselves unless they lead to suicidal thoughts and actions. If metabolomics can be used to identify the people at greatest risk, it could ultimately help us save more lives.”
The study was published in Translational Psychiatry.






