Cancer, an insidious disease that knows no bounds, is one of the leading causes of death worldwide. In 2020, cancer was responsible for nearly 10 million deaths, or nearly one in six deaths. While medical advancements have significantly improved cancer treatment and prognosis, there is still much scientists don’t know about how the immune system battles cancer. But this also means there are a lot of opportunities.
In a new study that may prove highly impactful, scientists at Cardiff University discovered a new type of killer T-cells in patients who had survived cancer and flushed out the disease from their bodies.
These highly potent T-cells, known as ‘multipronged’ T-cells, have superior capabilities to the traditional T-cells previously known to science, enabling them to recognize and attack multiple different cancer cells simultaneously.
Killer T-Cells and supercharging the immune system to fight cancer
T-cells are a type of white blood cell that play a pivotal role in the immune system’s defense against infections, foreign invaders, and abnormal cells, including cancer cells. These specialized cells are produced in the bone marrow and mature in the thymus gland, which is why they are called “T” cells.
There are two main types of T-cells:
- Helper T-Cells (CD4+ T-cells): These cells are responsible for coordinating the immune response. They assist other immune cells in identifying threats, activating killer T-cells, and stimulating B cells to produce antibodies against pathogens.
- Killer T-Cells (CD8+ T-cells): Killer T-cells are the frontline warriors in the immune system. Once activated, they can recognize and directly attack infected or cancerous cells, destroying them and preventing further spread.
Cancer cells often arise in our bodies as a result of mutations or other genetic abnormalities that cause them to grow uncontrollably. Normally, our immune system is equipped with a process called “immunosurveillance,” wherein immune cells, particularly T-cells, actively identify and eliminate these abnormal cells before they can develop into full-blown cancer.
However, cancer cells can sometimes evade detection and destruction by the immune system, allowing tumors to grow and spread. This evasion can occur through various mechanisms, including downregulating the expression of molecules that T-cells recognize or producing immunosuppressive substances that hinder T-cell activity.
But scientists aren’t sitting idle. The discovery that cancer cells can dupe our immune system into thinking there’s no threat has led to the development of a novel field of research called cancer immunotherapy. This field aims to enhance the body’s natural ability to fight cancer by boosting the immune response.
In practical terms, this can take the form of various therapies. For instance, Chimeric Antigen Receptor (CAR) T-cell therapy involves modifying a patient’s T-cells in the lab to express special receptors called CARs. These receptors enable T-cells to recognize and target specific proteins on the surface of cancer cells. Once infused back into the patient, CAR-T cells can effectively hunt down and destroy cancer cells.
Special T Cells
Similarly, tumor-infiltrating lymphocyte (TIL) therapy involves extracting white blood cells from a patient’s tumor, growing them in a laboratory, and reintroducing them into the patient to help the immune system combat the cancer cells.
In the new study, the Cardiff researchers analyzed the results of 31 patients in Denmark who received TIL therapy using T-cells over the span of a decade.
After identifying cancer survivors who showed strong killer T-cell responses to their own cancer over a year after clearance, the researchers analyzed the T-cells to understand how they distinguished cancer cells from normal cells. By utilizing algorithms, they successfully predicted which targets the cancer-specific T-cells recognize, based on the T-cells’ reactions and known differences in proteins between healthy and cancerous cells.
Much to everyone’s surprise, the scientists found that the T-cells from the cancer survivors could recognize multiple protein changes in cancer cells at once. In contrast, run-off-the-mill T-cells can only target one protein at a time.
These findings are groundbreaking, highlighting the potency of the ‘multipronged’ T-cells in recognizing cancer cells. Moreover, they suggest that such T-cells could respond to most types of cancer, as cancers only needed to express one of the abnormal targets to be identified as dangerous and destroyed.
Another noteworthy implication is that the presence of such T-cells could signify complete remission, offering much-needed solace to the patients.
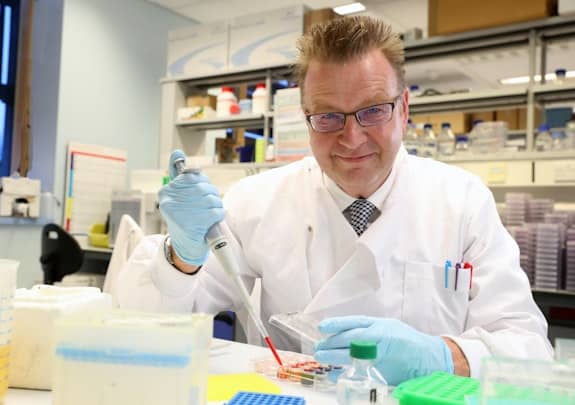
“Importantly, we have seen large numbers of multipronged T-cells in the blood of cancer survivors. To date, we have not found such multipronged T-cells in people where cancer progresses. Patient numbers are small so far, but it remains possible that multipronged T-cells might be associated with complete remission – or cancer clearance,” said Professor Andy Sewell of Cardiff University’s School of Medicine who led the research.
Engineering T-cells for future treatment
While the research is promising, more extensive studies on larger groups of patients are needed to establish a definitive link between multipronged T-cells and cancer clearance. Successfully predicting what a T-cell recognizes is a significant challenge in cancer research, but it holds immense potential to improve future cancer treatments.
Dr. Garry Dolton, one of the lead authors of the study, points out that they have seen multipronged T-cells in multiple cancer survivors. Their next step will be to investigate whether these cells are linked to a good prognosis.
Additionally, they hope to explore the possibility of genetically engineering this type of T-cell in the laboratory for use in treating a wide range of cancers, similar to how CAR-T cells are currently employed in treating some forms of leukemia. However, it’s essential to note that this research is still in its early stages and will take several years to progress.
The findings appeared in the journal Cell.






