Malaria is a disease of the most vulnerable: the very young and the poor. Every year, there are about 219 million cases of the disease, and more than 400,000 deaths every year. We can put and end to it.
The key to eradicating malaria is stepped up research and development of new tools to battle the disease, claims a World Health Organization (WHO) expert group that spent the last 3 years studying the trends and future projections for the factors and determinants that underpin malaria. The group, called the Strategic Advisory Group on Malaria Eradication (SAGme), published a 20-page executive summary of their report including a set of recommendations, ahead of a WHO-hosted malaria forum in Geneva on Sep 9.
Malaria infections and deaths have held steady since 2015, but there isn’t enough progress against the disease to achieve the 2030 goal set out in the latest WHO malaria strategy — cutting cases and deaths by 90%.
When the group looked at funding, they found that less than 1% of the support for health research targets tools to fight malaria. The group estimates that scaling up current interventions could prevent 2 billion more malaria cases and 4 million deaths by 2030, but only if they reach 90% of the population in countries that make up 95% of the global burden.
This could actually save money in the long run. The researchers calculated that the cost of the scale-up would be $34 billion and that the economic gain would be about $283 billion in total gross domestic product — putting the benefit-to-cost ratio above 8:1.
SAGme experts say it is theoretically possible to wipe out malaria, but not with the current control methods being used. Most tools used to battle the disease were developed in the past century or earlier. Promising new efforts are being developed, and the world’s first vaccine against malaria—RTS, S/AS01—has been deployed in Ghana, Malawi, and Kenya.
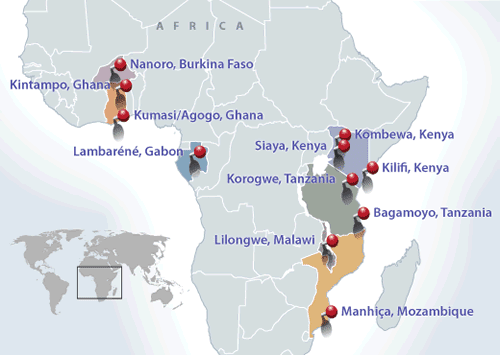
“An effective vaccine is something we desperately need if we’re ever going to get malaria under control and we just don’t have it,” said Professor Alister Craig, dean of biological sciences at the Liverpool School of Tropical Medicine. GSK and the Bill & Melinda Gates Foundation supported the development of the RTS, S/AS01 vaccine at a cost of ~$700 million. The effort culminated in 2015, when a study of about 15,000 subjects found that giving four doses of RTSS over 18 months cuts the number of malaria episodes that young children experienced by 36%.

SAGme also pointed to an urgent need to step up research and development and strengthen the pipeline, noting that a research agenda published in 2017 serves as a starting point.
A major challenge in many countries is access to health services. For example, only one in five pregnant women in moderate- to high-transmission parts of Africa can get drugs to protect themselves from malaria. Only half of those at risk for malaria on the continent sleep under insecticide-treated bed nets, and only 3% are protected by indoor insecticide spraying.
Expansion of the universal healthcare coverage and strengthening of health services are crucial so more people can access malaria prevention, diagnostics, and treatments. Better data on malaria transmission is also needed and better tools to control mosquitoes and protect and treat people in malarial regions.






