Although they’re relatively old technology in this day and age, there is renewed interest in iron lungs today against the backdrop of the coronavirus pandemic.
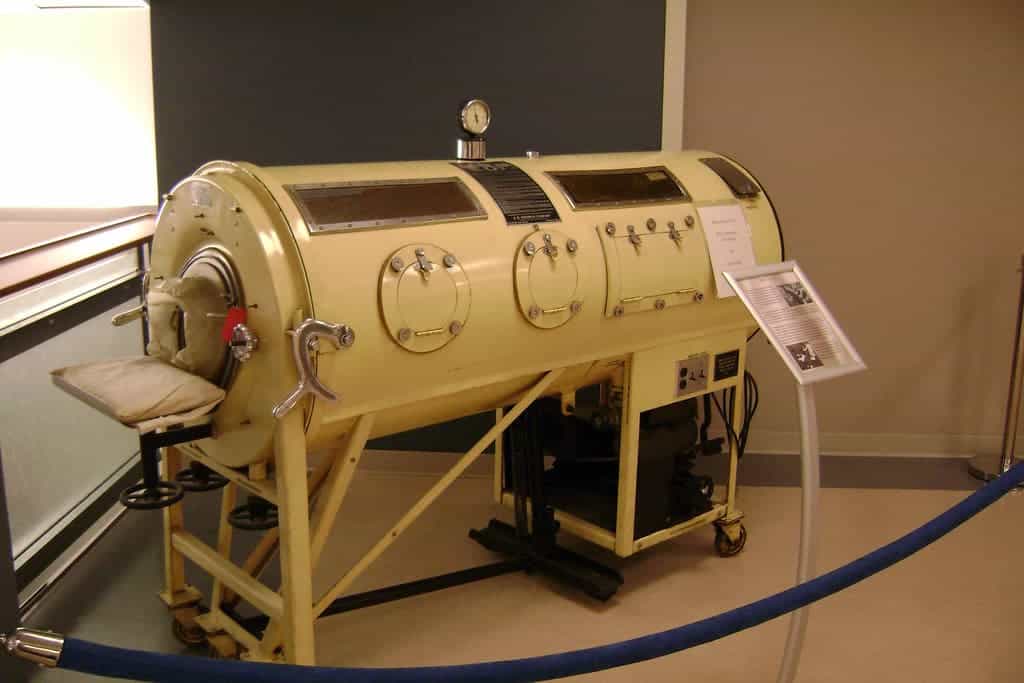
Few devices can boast having as terrifying — and cool — a name as the iron lung. These somewhat outdated medical devices were the earliest devices designed to help patients breathe. Compared to modern breathing aides, these devices were huge and quite scary-looking.
Still, iron lungs were a very important development at their time. In the aftermath of the COVID-19 epidemic, there has also been renewed interest in these devices as they can be used as an alternative to modern ventilators.
So let’s take a look at exactly what iron lungs are, and how they came to be.
So what are they?
Iron lungs are quite aptly named; unlike other modern ventilators, they function using the same mechanisms as our own lungs.
An iron lung is a type of negative pressure ventilator. This means that it creates an area of low-pressure or vacuum to move and draw air into a patient’s chest cavity. In very broad lines, this is the exact mechanism our bodies employ, via movements of the diaphragm, to let us breathe.
The concept behind these devices is quite simple. The main component of an iron lung is a chamber, usually a metal tube (hence the ‘iron’ part in its name) that can fit the body of a patient from the neck down. This acts as an enclosed space in which pressure can be modified to help patients breathe. The other main component of the device is mobile and actually changes the pressure inside the tube. Usually, this comes in the form of a rubber diaphragm connected to an electrical motor, although other sources of power have been used, including manual labor.
Patients are placed inside an iron lung, with only their head and part of their neck (from their voice box upwards) left outside the cylinder. A membrane is placed around their neck to ensure that the cylinder is sealed. Afterward, the diaphragm is repeatedly retracted and contracted to cycle between low and high pressure inside the chamber. Because the patient’s head and airways are left outside of the cylinder, when pressure is low inside it, air moves inside the patient’s lungs. When pressure increases inside the cylinder, the air is pushed back out.
The whole process mirrors the way our bodies handle breathing. Our diaphragm muscles draw on the lungs, increasing their internal volume, which pulls air in from the outside. To breathe out, the diaphragm muscle squeezes on the lungs, pushing air out. Iron lungs work much the same way, but they expand and contract the lungs alongside the rest of the chest cavity from outside the body.
This process is known as negative pressure breathing; low (‘negative’) pressure is generated in the lungs in order to draw in air. Most modern ventilators work via positive pressure: they generate high pressure inside the device to push air into the patient’s lungs.
One advantage of such ventilators is that patients can use them without being sedated or intubated. On the one hand this eases the pressure on medical supplies each patient requires; on the other, it slashes the risks associated with the use of anesthetics — such as allergic reactions or overdoses — and the risk of mechanical lesions following intubation.
Epidemics, pandemics

“The desperate requests for ventilators in today’s treatment of patients in the grasp of the coronavirus brought to mind my encounter with breathing machines in the early 1950s polio epidemic, when I signed up as a volunteer to manually pump iron lungs in case of power failure at Vancouver’s George Pearson Centre,” recounts George Szasz, CM, MD, in a post for the British Columbia Medical Journal.
Iron lungs saw their greatest levels of use in developed countries during the poliomyelitis outbreaks of the 1940s and 1950s. One of the deadliest symptoms of polio is muscle paralysis, which can make it impossible for patients to breathe. The worst cases would see patients requiring ventilation for up to several weeks. Back then, iron lungs were the only available option for mechanical ventilation, and they saved innumerable lives.
As technology progressed, however, iron lungs fell out of use. They were bulky and intimidating machines, hard to transport and store despite their reliability and mechanical simplicity. With more compact ventilators, the advent of widespread intubation, and techniques such as tracheostomies, such devices quickly dwindled in number and use. From an estimated height of around 1,200 iron lung devices in the U.S. during the ’40s and ’50s, less than 30 are estimated to still be in use today
There are obvious parallels between those polio epidemics of old and today’s COVID-19 pandemic in regards to the need for ventilation. Machines such as the iron lung have been suggested as a possible treatment option for COVID-19 patients due to this. For most cases, such devices can help, but not for all.
In cases of severe COVID-19 infections, the tissues of the lungs themselves are heavily affected. A buildup of fluid in the lungs can physically prevent air from reaching the alveoli (the structures in the lung where gases are exchanged between the blood and the environment). While iron lungs can perform the motions required to breathe even for patients who are incapable of doing it themselves, they cannot generate enough pressure to push air through the tissues affected by a COVID-19 infection.
“Iron lungs will not work for patients suffering from severe COVID-19 infections,” explains Douglas Gardenhire, a Clinical Associate Professor and Chair of Respiratory Therapy at the Georgia State University (GSU) Department of Respiratory Therapy. “Polio interrupted the connection between brain and diaphragm and while some polio patients did have pneumonia, it was not the principal issue. For the most part, the lungs themselves did not have any change in their dynamic characteristics.”
“COVID-19 pneumonia physically changes the composition of the lungs,” adds Robert Murray, a Clinical Assistant Professor at the GSU. “The consolidation of fluid in the lungs will not respond with low pressure generated by the iron lung. The lungs of a COVID-19 patient will be a heterogenous mix of normal and consolidated lung tissue making mechanical ventilation very difficult.”
Still an alternative
Although patients with severe COVID-19 infections might not benefit from the iron lung, there are cases in which the device can prove useful. One paper (Chandrasekaranm, Shaji, 2021) explains that there still is a need for negative pressure ventilators in modern hospitals, especially for patients who have experienced ventilator-induced lung injuries. The use of negative pressure ventilators, especially in concert with an oxygen helmet, may also play a part in reducing the number of infections by limiting the spread of viruses through contaminated materials in cases where resources are stretched thin, the team adds.
While the concept is being retained, however, the actual devices are getting an upgrade. One example is the device produced by UK charity Exovent, which aims to be a more portable iron lung. Exovent’s end goal is to provide a life-saving device that will impose fewer limits on what activities patients can undertake. A seemingly-simple but still dramatic improvement, for example, is that patients can use their hands to touch their faces even while the Exovent device is in operation. Eating or drinking while using the device is also possible.
Exovent’s ventilator was designed before the coronavirus outbreak to help the millions of people suffering from respiratory issues including pneumonia worldwide. However, its designers are confident that, in conjunction with oxygen helmets, it can help patients who are recovering from a coronavirus infection — a process that leaves them with breathing difficulties for months.
All things considered, iron lungs have made a huge difference for the lives of countless patients in the past, and they continue to serve many. Although most of them today look like archaic devices, engineers are working to update and spruce them up for the modern day. And, amid modern ventilators, there still seems to be a role — and a need — for devices such as iron lungs.


