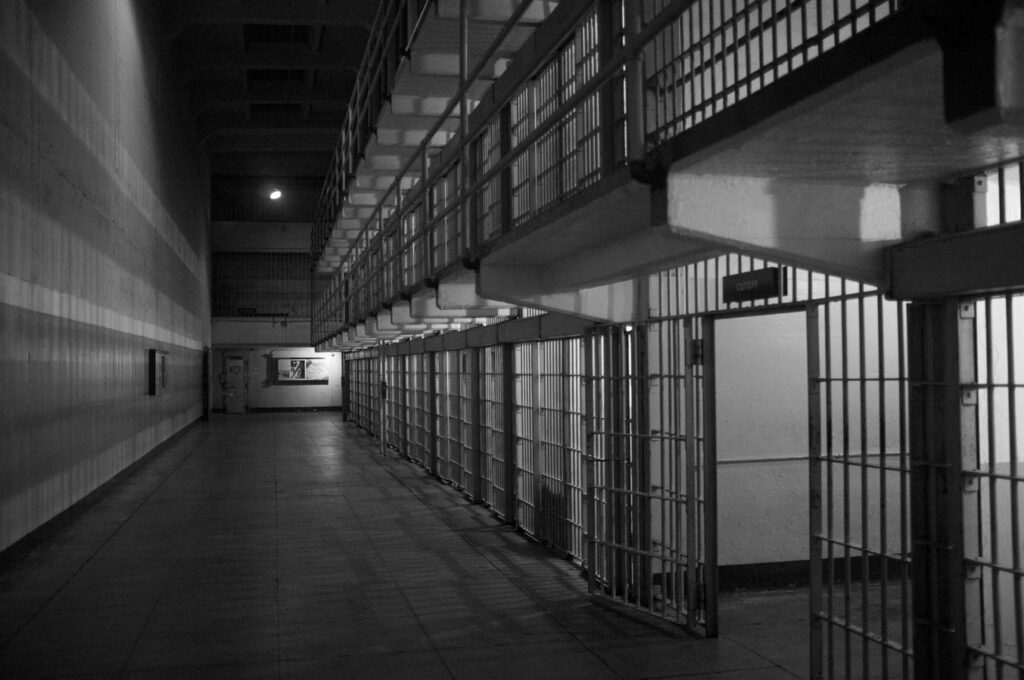
Without measures to mitigate the spread of COVID-19 in prisons, the disease could wreak havoc — especially in the US.
The United States has the highest documented incarceration rate in the world: 75 out of every 10,000 people (or 0.7% out of the entire population) are incarcerated. The US, which accounts for around 4% of the world’s population, houses 22% of the world’s prisoners. In total, over 2.3 million people are behind bars, with the number increasing 500% in the last 40 years, despite crime steadily dropping at the national level.
That means that 2.3 million people are at a very high risk of COVID-19 infection.
Prisons and disease
It wouldn’t be the first time a pandemic devastates prisons, write three researchers in a viewpoint for the medical journal JAMA. In 1918, for instance, the Spanish Flu brought chaos to all the prisons it penetrated. An account from San Quentin prison detailing the Spanish influenza of 1918 estimated that half of the 1900 inmates contracted the disease during the first wave of the epidemic. Sick calls increased from 150 to 700 daily and contrary to protocol, most of the ill were kept in the general prison population because the hospital ward was full.
To make matters even worse, the population in prisons is increasingly gentrified. As a result of longer sentences (mostly for non-violent offenses), the average age of the prison population has increased substantially. In 2013, state prisons housed 131,500 people over 55 years, a 400% increase since 1993. Many incarcerated persons older than 55 years have chronic conditions, such as heart and lung diseases, putting them in the highest risk categories for COVID-19.
In addition to being crowded, few US prisons have health systems capable of accommodating a surge in sick calls. If something similar to the Spanish influenza situation at the San Quentin prison were to happen, there would be little support to be offered to prisoners. Although the US Constitution guarantees a right to healthcare for those who are incarcerated, in practice, this is unlikely to be ensured should COVID-19 cases in prisons start to increase. Incarcerated persons may even be charged co-payments that are very high relative to the little revenue they generate, which will deter many from seeking care.
Meanwhile, prisons are supporting the US coronavirus effort through prisoner work.
Working through a pandemic
New York Gov. Andrew Cuomo announced on March 9 that the state prison system’s industrial arm, Corcraft, would help produce hand sanitizer. Other states quickly followed. Incarcerated populations were put to work washing potentially contaminated hospital laundry; manufacturing protective equipment; disinfecting cleaning supplies; and digging mass graves. Nearly every US state has some sort of program where incarcerated populations are contributing labor to the pandemic response, and the pay is almost negligible.
The pay for such work is, on average, between US$0.14 and $0.63 an hour, and some states (such as Alabama, Arkansas, Florida, Georgia, and Texas) don’t pay wages at all for this work. This is partially addressed in some states, for instance in New York, where gravediggers are paid $6 an hour.
But the way the work itself is being carried does not seem to respect social distancing measures. The Arkansas Department of Corrections recently posted an image of incarcerated workers making masks while sitting next to one another, which has been taken down now. A video posted on April 7 showed incarcerated women in Arizona making masks, without wearing any gloves and sitting inches apart from each other.
Meanwhile, in Pennsylvania, prison manufacturing ramped up, with incarcerated people working 12 hours a day, 6 days a week to produce masks, antibacterial soap, medical gowns, and disinfectant (although the standard workday for incarcerated workers is 6 hours a day).

Exposure and risk
Even before the COVID-19 outbreak, clinicians and advocates called for better health conditions in prisons. When it became clear that COVID-19 would become a pandemic, many looked at prisons as extremely vulnerable places and proposed precautionary measures, such as making protective equipment widely available, eliminating the medical co-payments and other disincentives, and providing appropriate medical care for incarcerated people.
Few of these things happened.
In Missouri, incarcerated workers are continuing to wash and handle hospital laundry, raising the risk of bringing outside infection to prisons, and this is hardly an isolated arrangement. Prisons provide important labor at low costs, but the occupational hazards that go along with this are generally ignored, as is the CDC guidance on managing coronavirus in detention facilities. If COVID-19 enters prisons, it will spread like wildfire — and we are already seeing this starting to happen.
However, the Harvard researchers writing the JAMA viewpoint say that no matter how you go about it, the bottom line is that prisons are just too crowded to be safe in the face of a disease such as COVID-19.
“[T]he most effective way to avoid an imminent outbreak, is, as others have argued, to drastically reduce the populations of jails and prisons. Criminal justice systems can accomplish this by reducing unnecessary jail admissions and expediting prison release. Some prosecutors are already adjusting prosecutorial standards to reduce jail admissions and the length of stays.”
Some steps have been taken to reduce crowding in some jails (for instance, the prosecution of drug possession and other minor crimes is being deterred in some cities), but overall, most prisons and jails remain unaffected.
Every day, the number of incarcerated persons and prison workers who have tested positive for COVID-19 grows, with few clear solutions in sight.


