A British study used a symptom-tracing app and machine learning to group the most common COVID-19 symptoms. The researchers also assessed how likely it is for each type of symptom to lead to a severe case.

A tracing app shows its worth
It’s estimated that over 4 million people use the Covid Symptom Tracker app. The app is meant to serve as a tracker to see how coronavirus cases are changing through different communities, and also to learn about the symptoms associated with COVID-19.
Any information can be life-saving, and we’ve already seen that the virus can be extremely unpredictable. Symptoms can range from diarrhea and confusion to chest pain and extreme fatigue, but we’re still not sure just how common these symptoms are, and how likely they are to indicate that something bad is coming. Knowing whether someone is likely to require ventilation a couple of days in advance could make all the difference, both for hospitals (who can prepare accordingly) and for the patients themselves.
In the study, the team used a machine learning algorithm to explore whether symptoms can be clustered together. Overall, the team drew data from 1,653 users who tested positive and regularly noted their symptoms and health situation. Out of them, 383 went to the hospital at least once, and 107 required either extra oxygen or ventilation. According to the researchers, the symptoms can be clustered together, and they can be used to assess the likelihood of a severe case.
The key is to take several symptoms together.
“As no one symptom can predict disease severity or the need for dedicated medical support in COVID-19, we asked if documenting symptom time series over the first few days informs outcome,” the authors write.
The six categories of coronavirus symptoms
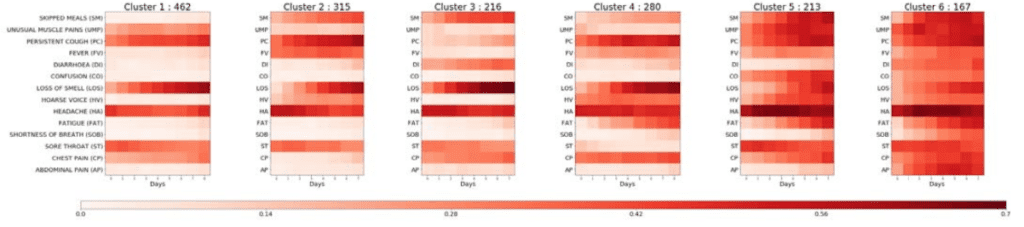
After the researchers gathered the data from the patients, they fed it into an unsupervised machine learning algorithm that clustered the groups of symptoms together. The six clusters of symptoms that researchers found are:
- Cluster 1 — largely upper respiratory tract symptoms (especially persistent cough). Muscle pain was also present. Around 1.5% of patients in this cluster required respiratory support, and 16% made at least one visit in the hospital. This was the most common cluster.
- Cluster 2 — largely upper respiratory tract symptoms, but a greater frequency of skipped meals, and higher fever. In this group, 4.4% required respiratory support, and 17.5% visited the hospital.
- Cluster 3 — gastrointestinal symptoms (such as diarrhea), but surprisingly, fewer other symptoms. Here, 8.6% required respiratory support, and 23.6% made at least one trip to the hospital.
- Cluster 4 — early signs of fatigue, severe chest pain, and persistent cough. Out of this cluster, 8.6% required respiratory support and 23.6% went to the hospital.
- Cluster 5 — confusion, severe fatigue, and many skipped meals. Out of this group, 9.9% required respiratory support, and 24.6% visited the hospital.
- Cluster 6 — respiratory distress, including breathlessness and chest pain, in addition to fatigue, confusion, and gastrointestinal problems. Almost 20% required respiratory support, and 45.5% went to the hospital at least once.
Researchers also note that a higher body mass index correlated with more severe symptoms, as did older age and chronic lung disease. Men were also more likely to report severe symptoms.
The first two clusters were associated with milder forms of the disease. The third one was rather unusual, since the symptoms tended to manifest at the gastrointestinal level, instead of the respiratory one. Then, the other clusters get progressively worse. Clusters 5 and 6 were at the greatest risk of hospitalization and were most likely to require artificial ventilation. Clusters 3 and 4 also had a relatively high risk.
If widely utilized, this could offer healthcare providers important information. It could allow patients to be monitored remotely and help predict how many hospital beds and ventilators would be needed in the near future.
The team says the findings could give healthcare providers several days advanced warning of demand for hospital care and respiratory support.
It could also help flag patients at risk of becoming seriously ill, directing home support such as an oxygen meter or nurse visits. At present, the authors write, the average time to get to hospital is 13 days.
However, the study should also be taken with the grain of salt. The sample size only included a few hundred patients for each cluster, which may not be enough to get an accurate picture of what is going on. The clustering itself was done by an algorithm merely by association — this is more an indication than a clear symptom classification. Lastly, the study has not been peer-reviewed and is awaiting expert analysis.
Nevertheless, as we gather more and more pandemic data, it is becoming increasingly clear that the picture is far from clear, and data is often confusing or inconclusive. It is this type of classification that could help us better understand the disease and how to prepare local hospitals.
If this study is confirmed, it could save lives.
The study has been published on medRxiv.