It was the year 1347 when Genoese traders unwittingly brought a new disease from Asia to the ports of Europe. It was called the Pestilence initially, ultimately being known as the Black Death or the Black Plague.
The pandemic lasted for four years until 1351, and killed between 75 and 200 million people. At the time, the world population was estimated to be around 400 million people, so nearly half of the world’s population was wiped out within a few years. If we were to bring it to today’s population, that would be over 3 billion people dying in the next few years due to a single disease.
The Black Death pandemic is possibly the most tragic moment in human history, way worse than any other disease, famine, or war.
Nearly 700 years later, the world is crippled by a new virus, SARS-CoV-2, which has already infected millions and caused the death of hundreds of thousands. COVID-19 — the disease caused by the novel coronavirus — has put most of the world under lockdown, with many people being forced to stay at home for weeks or months to avoid the spread of the virus. It is estimated that, if no measures were taken, millions of people would have died already of this new disease, which has a mortality rate estimated by the World Health Organization (WHO) of around 3.5%.
Of course, we don’t have it quite as bad as with the Black Plague.
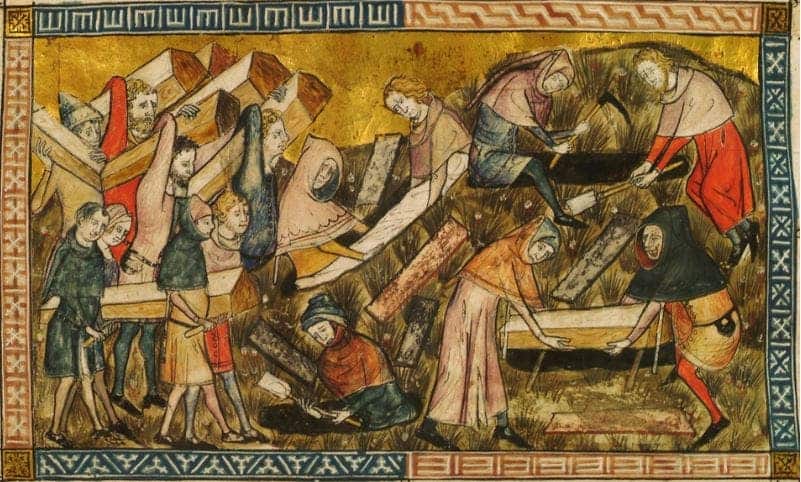
From 1347 until 1351, the situation was much worse than it is now. Without any viable treatment, people were dying at home after experiencing vomiting, diarrhea, bleeding, and extremely swollen lymph nodes — few doctors were brave enough to attempt to save lives, given the extremely high risk of getting infected themselves. People would lock themselves at home and leave only if strictly necessary. And many still died. Mothers abandoned their children, and families became separated. Without effectively any rulership, cities were left in anarchy, with dangerous rituals, plundering, and violence abundant.
Of course, our knee jerk reaction to that is to think that it couldn’t possibly happen now.
Before the coronavirus pandemic arose, most people believed we had developed a society that was medically and technologically prepared for any kind of epidemic. Whatever was thrown our way, we could handle it — that seemed to be the general state of mind.
But the Western world, largely safe of infectious diseases, severely underestimated the dangers posed by contagious diseases, such as Ebola, spreading in poorer regions of the world. Many were tempted into believing that these diseases are still around only because some countries are so heavily underdeveloped that they don’t have sufficient medical technology, equipment, or even knowledge to control them.
Yet, as the coronavirus pandemic has revealed so far, infectious diseases can pose major health risks in all parts of the world.
The coronavirus pandemic is teaching the world that we are all susceptible creatures and our medical know-how doesn’t necessarily provide an immediate solution against an epidemic disease of this caliber. After months of pandemic, we are still left with no cure and no preventive system — and progress is slow and tedious. Just like in medieval times, one of our best bets is social distancing.
When we think of the Black Death, we think of the Middle Ages as a time of despair, lacking in medical and social knowledge. However, this is mostly a historical misconception. We must ask ourselves if diseases such as plagues can constitute a threat today as they have done for hundreds of years.
The plague is still around
The plague exists in three forms — the pneumonic, the septicemic, and the bubonic form. The Black Death of the 14th century was of the bubonic type.
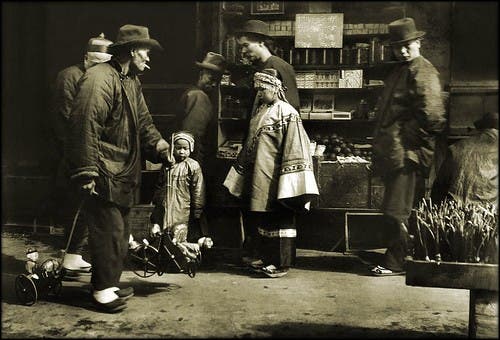
The plague is caused by a bacterium called Yersinia pestis, named after and discovered by Alexandre Yersin, who studied the bubonic plague outbreak in Hong Kong in 1894 (1894 certainly isn’t the Middle Ages). Yersin discovered that the bacillus could spread in humans and rats. Later, other scientists identified the intermediate host. As with COVID-19, which likely originated in bats and possibly reached humans via pangolins, Y. pestis also passed from rats to humans via another host, the oriental rat flea.
Of course today, the plague doesn’t affect us as much because we have antibiotics.
The discovery of antibiotics, thanks to the work of Alexander Fleming in the first half of the 20th century, is widely considered as one of the biggest medical achievements of all time. Following the 1347 Black Death pandemic, plague outbreaks continuously repeated throughout human history until Fleming’s groundbreaking discovery of penicillin. To name the most recent outbreaks, the third plague pandemic started in China around 1855 and within a few years killed 12 million people, mostly in India. Minor outbreaks occurred in China (1865), Hong Kong (1894), and San Francisco in the US (1900 and 1907).
Antibiotics have proven very effective against Y. pestis. The mortality rate of bubonic plague, the most severe form, is between 40 and 80% if left untreated, but antibiotics can reduce it to less than 10%, which is still nearly three times higher than the COVID-19 case mortality rate when untreated. To avoid death caused by bubonic plague, patients have to be treated with antibiotics within 24 hours of the first symptoms. When people die from the disease or manifest the symptoms, prompt medical intervention consists of the administration of prophylactic antibiotic treatment to all those who could have been in contact with the bacterium, and this is what prevents outbreaks from becoming pandemics.
Following the introduction of antibiotics in our daily lives, the recurrence of plagues drastically slowed down. According to the World Health Organization, the pandemic was considered active until 1959, when worldwide casualties dropped to 200 per year.
But the plague never really went away.
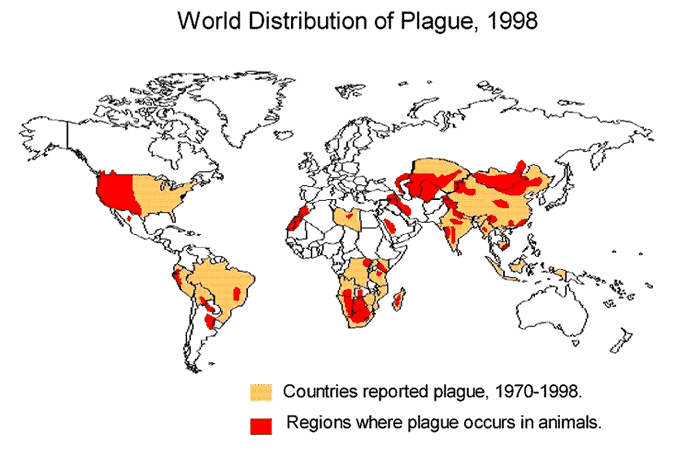
In recent times, various outbreaks of bubonic plague emerged in Madagascar between 2012 and 2017, with 2017 being the deadliest outbreak in the country with 124 confirmed deaths. Other cases have appeared in the past 20 years in the Democratic Republic of Congo (with more than a thousand cases recorded) and also in India, China and Peru, among others. The United States confirmed that a child was infected in Idaho in 2018, the first case in a long time.
Although the plague has never really abandoned us, for most people the existence of an efficient cure based on antibiotics — corroborated by the existence of a vaccine (functional but seemingly not very efficient) — is enough to consider these cases isolated and to classify Y. pestis as a disease of the past.
However, antibiotics are increasingly revealing themselves to be more of a temporary medical solution for mankind. They have been considered a medical miracle for the past century, but miracles tend to be short-lived in science.
Bacteria can indeed adapt and find alternative strategies to infect their hosts. Antibiotics put bacteria under strong selective pressure. If within a population of bacteria, one or more of them, by chance, possesses a mutation that makes it insensitive to a given antibiotic, the bacterium will divide and initiate a new population that is not susceptible to the antibiotic. This is what in medicine is called “antibiotic resistance”. Each time a human being or an animal is given antibiotics, we are increasing the odds of generating super-resistant bacteria.
For this reason, old diseases will likely reappear sooner or later, if no solutions are at hand. And most of all, we need to be careful with the deadliest disease of all time, the Black Death.
In Madagascar, strains of Y. pestis responsible for the plague that were resistant to some types of antibiotics were isolated from patients, and in particular one multi-resistant strain for all the antimicrobial drugs used for treatment was isolated in 1995. Although these can still be treated with other antibiotics, the list of functional treatments is becoming rather short, and we may incur new resistances in the future. It follows that the emergence of known resistance in this deadly bacterium is of great concern.
Even more concerning is the origin of the antibiotic resistance of Y. pestis. It turns out that these bacteria may exchange genetic information in a process known in microbiology as “horizontal transfer”. Basically, bacteria of different types, if in close proximity, may exchange plasmids, which are circular pieces of DNA.
Antibiotic resistance
The flea, which is the vector of transmission between rodents and humans, has a digestive system that contains various bacteria including Escherichia coli. This bacterium has developed multi-drug resistance over the past decades, due to it being treated with antibiotics because of its role in various diseases such as traveler’s diarrhea, urinary tract infection or pneumonia. Therefore, the most plausible explanation is that the digestive flora of fleas could have transmitted genetic information to Y. pestis, causing the emergence of resistant strains.
It is therefore possible that the world could be getting increasingly exposed to a modified form of the bacterium, which in its non-resistant form wiped out nearly half of the world’s population in the 14th century, and killed many more in the following centuries.
Currently, powerful antibiotics are our protective shield against this disease, assisted by practices of good hygiene. But cleaning our hands with soap – as for the coronavirus – isn’t enough. We need treatment solutions. Research is needed to prevent a pandemic that would be devastating for humanity.
Ethics and bioweapons
Hope is kindled by potential alternative treatments such as “phage therapy”, which involves the use of bacteriophages – viruses that infect bacteria – being designed and genetically manipulated to specifically target a pathogenic bacterium, such as Y. pestis. Already known bacteriophages for Y. pestis exist, and even multi-resistant forms of these bacteria can be specifically targeted and killed. There are however drawbacks to this approach, and this we shouldn’t think we’re out of the woods just yet, at least until these solutions are truly at hand.
Our immune system fights against any foreign intruder, as it does against the coronavirus. It would therefore also fight any other virus, even if we deliberately infected ourselves in order to kill bad bacteria. In other words, our immune system would try to defend our bodies from what should actually be defending us from the bacteria. In addition, even these beneficial viruses may produce toxins. And finally, bacteria may develop resistance to bacteriophages, as these are very specific to a particular bacterium. Most of the time this won’t be a problem, as bacteriophages target essential components of bacteria that are necessary for their function. However, the concern remains that bacteria may develop resistance to both antibiotics and bacteriophages.
Ethical arguments are also slowing down the development of effective bacteriophages for the treatment of many infectious diseases, and the world is increasingly looking with suspicion at scientists playing with viruses, even if this is ultimately for our own benefit. And these arguments should be considered, because together with its benefits, science has always brought dangers, too.
In the case of antibiotics, we haven’t realized quickly enough that nature finds a way through, sooner or later. And we must win this race mankind is playing against nature, finding new treatments before infectious agents adapt to the old ones. At the same time, we must be concerned about creating dangerous organisms, increasing the risk they are mishandled or even used as bioweapons. This could very well happen with Y. pestis too.
For the plague, so far the preventive focus has been to target those countries with endemic plagues such as Madagascar, the Democratic Republic of Congo and Peru. However, if the COVID-19 pandemic is teaching us something, it’s that the West isn’t immune to pandemics, and actually could be even more exposed, because of the ease of circulation of goods and people, tourism, incessant international business — and perhaps also because of the misconception that we are well-prepared to face any kind of threat.
We should all consider Y. pestis as a resurgent threat for our civilization, and we should invest all our efforts into preventing a plague pandemic. Overpopulation, climate change and famine make this world a perfect place for a devastating disease. A new Black Death pandemic may be on the horizon, and we need to avoid it.
Here you find a list of scientific papers discussing the topic:
- Galimand, et al. “Resistance of Yersinia pestis to antimicrobial agents”, Antimicrobial Agents and Chemotherapy, 2006
- Ditchburn and Hodgkins, “Yersinia pestis, a problem of the past and a re-emerging threat”
- Welch et al., “Multiple Antimicrobial Resistance in Plague: An emerging public health risk”, PLOS ONE, 2007
- Galimand et al., “Multidrug resistance in Yersinia pestis mediated by a transferrable plasmid”, The New England Journal of Medicine, 1997.
Federico Germani is a geneticist and molecular biologist at the University of Zurich, Switzerland. He is the founder and director of Culturico. He can be reached on Twitter @fedgermani


