An old cell can learn new tricks!
New research reveals a surprising level of plasticity in pancreatic cells, which morph to maintain proper hormone levels in the blood. The findings suggest that many other specialised cells could hold this ability, pointing the way to new treatment options for conditions that involve massive cellular death.
Class reroll
“What we are showing here is that the state of differentiation of a given cell is not carved in stone. Cell identity, at all stages of life, is modulated by the immediate cellular environment, particularly by inhibitory signals,” says lead author Professor Pedro Herrera from the Université de Genève (UNIGE) Faculty of Medicine. “Cell identity maintenance is therefore an active process of inhibition throughout the life of the cell, and not an intrinsic or passive state of differentiation.”
“This ability of specialized cells to change their function could prove crucial for treating other pathologies that are due to massive or inappropriate cell death, such as Alzheimer’s disease or myocardial infarction”.
The research was born of the team’s interest in diabetes, a disease that involves damage or destruction (through various means) of insulin-producing cells in the pancreas. This dismantles our bodies’ ability to regulate blood-sugar levels, leaving an excess in the blood over long periods of time, which leads to all sorts of complications: blindness, kidney failure, heart attacks, stroke, to name a few. Onset of diabetes is strongly linked to lifestyle. According to the WHO, over 8.5% of adults worldwide suffered from diabetes (both types combined, figures for 2014) and roughly 1.6 million deaths were directly caused by diabetes in 2015. Needless to say, it’s a wide-reaching condition with a severe quality of life impact — so there is a lot of interest in finding a cure.
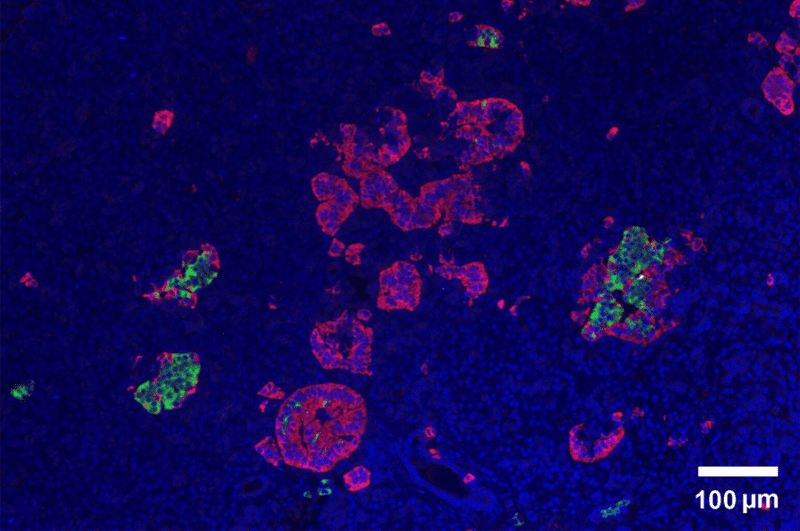
Pancreatic cells involved in blood-sugar regulation come in three flavors: α (alpha) cells which produce glucagon, β (beta) cells which produce insulin, and δ (delta) cells which produce somatostatin. These cells bunch together in small clusters known as pancreatic islets. Glucagon raises sugar levels in the blood, insulin works to reduce it, and somatostatin is the hormonal equivalent of a manager’s email, governing activity in the pancreas. Diabetes is characterised by the absence of functional β cells, taking away the pancreas’ ability of reining in blood sugar.
In a study published back in 2014, however, Herrera and his colleagues showed that some pancreatic cells can switch their role to supplement the production of insulin if push comes to shove. In mice without β cells, they reported at the time, new insulin-producing cells appear spontaneously. However, it’s not a huge number — only “1 to 2% of α and δ cells”, Herrera explains, — way too few to fix diabetes.
“Why do some cells do this conversion and others not? And above all, would it be possible to encourage it? These are the questions that are at the heart of our work,” Herrera adds.
To get to the bottom of things, the team analysed gene expression in pancreatic cells before and after the disappearance of β cells in pancreatic tissue. The first finding was that α cells suffer two key modifications: they start over-expressing some genes typically seen in β cells, and some that are characteristic for glucagon-producing α cells. Herrera’s team reports that insulin receptors on the surface of α cells suggests that their functions hinge on this hormone being present as well — hence, their activity is disrupted when β cells are destroyed.
Next, the team transplanted pancreatic islets into healthy mice to see what could coax these cells into morphing. Their hypothesis was that, when faced with hyperglycemia (high blood-sugar), α cells would change roles to address the lack of insulin.
In non-diabetic mice with functional β cells, and without hyperglycemia, some of the transplanted α cells started producing insulin when the β cells died in the grafted islets. This pretty much invalidated the team’s hypothesis, as a conversion was observed without hyperglycemia to act as a cue. The pancreatic environment itself was ruled out as a cause, too, as the grafts were placed in the renal capsule (i.e. outside of the pancreas). The only explanation, the team adds, is that the reprogramming capacity is intrinsic to the very pancreatic islet where these cells are located.
“Thus, in the same graft, only islets without β cells displayed reprogramming. No cell conversion occurred in neighbouring islets containing all their β cells,” says Herrera.
When the team blocked the insulin receptors of α cells in healthy mice, some of them started to produce insulin themselves — suggesting the hormone acts as a sort of ‘business as usual’ signal for α cells, preventing them from changing roles.
“By administering an insulin antagonist drug, we were able to increase the number of α cells that started producing insulin by 1 to 5%. In doing so, these cells became hybrids: they partially, but not fully changed their identity, and the phenomenon was reversible depending on the circumstances influencing the cells. Now that we are beginning to understand the mechanisms of this cellular plasticity, we believe that these adaptive cell identity changes could be exploited in future new treatments,” Herrera concludes.
While the work focused on pancreatic cells, there’s no reason why other specialised cells in the body couldn’t employ similar processes, the team says. More work will be needed to determine which cells can morph this way, and what would encourage them to do so — but, should we succeed, it could lead to new and very powerful treatments against conditions that involve cellular damage and death.
The paper has been published in the journal Nature Cell Biology.