Our current understanding of SARS-CoV-2 immunity is mainly based on previous experiences with SARS-CoV (2003) and recent studies in patients infected with and recovered from SARS-CoV-2 (2020).
Similar to the SARS-CoV infection, the main antibody targets in SARS-CoV-2 are the spike and nucleocapsid proteins (NCP) — and this is where the vaccines also strike. However, it’s not clear if lasting immunity against the novel coronavirus can be achieved because serum antibodies seem to decline. Since this pandemic is still relatively new, we haven’t had much time to explore just how long antibodies and immunity lasts — but new results are coming in.
Two new studies published recently demonstrate that COVID-19 antibodies last as long as 8 months, or potentially even more, giving some good news for a mass vaccination campaign.
A study published in Science Immunology followed a small cohort of Australians from day 4 to day 242 after infection. All patients demonstrated the presence of memory B cells — immune cells that “remember” viral proteins and can trigger rapid production of antibodies when re-exposed to the virus — as long as 8 months after the initial infection.
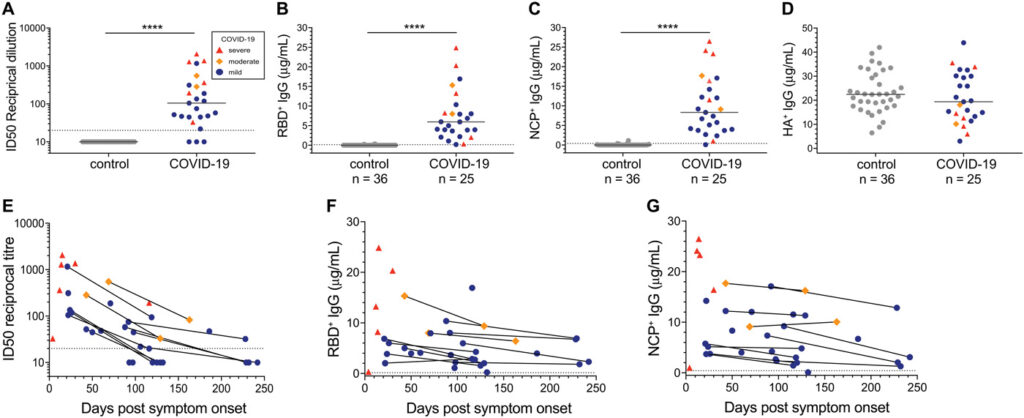
Researchers took blood samples from 25 confirmed COVID-19 patients with a range of disease severities and 36 healthy control patients from March to September, evaluating each patient’s antibody status and levels of virus-specific immune cells. The study showed that by day 6 post-infection, all patients showed immunoglobulin G (IgG) antibodies for the viral receptor-binding domain (a protein on the viral surface that binds to cell receptors, allowing entry and infection) and the nucleocapsid protein. The immunoglobulin G levels began declining 20 days after symptom onset. However, memory B cell levels continued to rise up to 150 days post-infection and remained detectable 240 days post-symptom onset, suggesting that patient immune systems were primed to respond to reinfection.
According to the authors, cellular immunity could explain why there are few documented cases of reinfection with SARS-CoV-2 and why immunity can last longer than the antibody levels would suggest it.
Another study investigated antibody responses in 58 confirmed COVID-19 patients in South Korea 8 months after asymptomatic or mild SARS-CoV-2 infection.
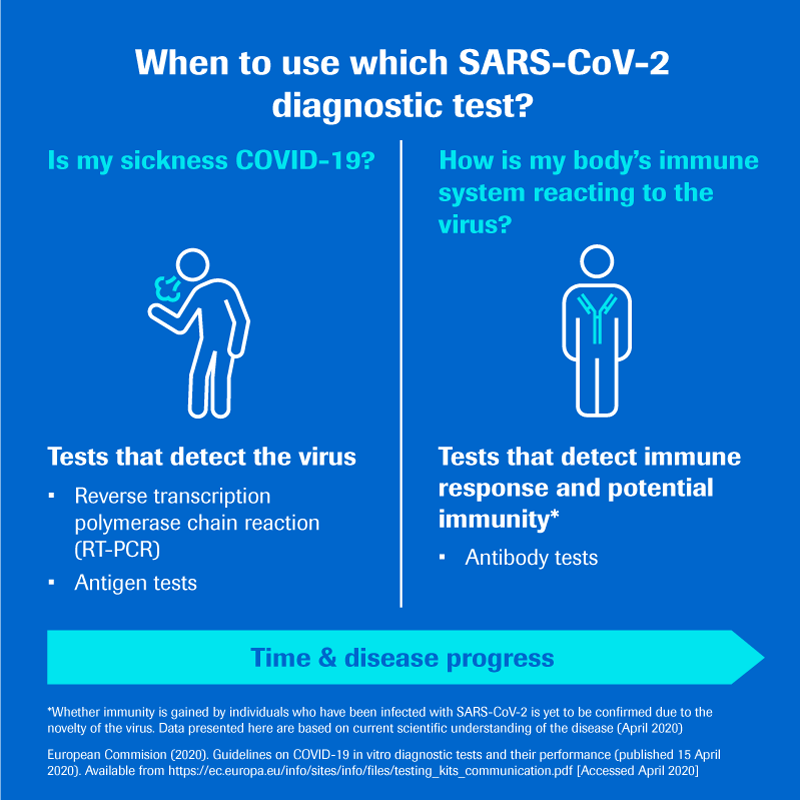
The team used 4 commercially-available immunoassays:
- an antinucleocapsid (anti-N) panimmunoglobulin (pan-Ig) electrochemiluminescence immunoassay (ECLIA) (Elecsys Anti-SARS-CoV-2 from Roche Diagnostics);
- an anti-N IgG ELISA (EDI Novel Coronavirus COVID-19 ELISA Kit from Epitope Diagnostics;
- an antispike (anti-S) IgG ELISA (SCoV-2 Detect IgG ELISA from InBios International);
- an anti-S1 spike subunit IgG ELISA (Anti-SARS-CoV-2 ELISA (IgG) from Euroimmun).
Except for the anti-N IgG ELISA, all of these immunoassays have been granted Emergency Use Authorization by the US Food and Drug Administration.
For 3 of 4 immunoassays used, seropositivity rates were high (69% to 91.4%; P < 0.01). These results, published in Emerging Infectious Diseases, are contradictory to both the first study’s antibody data and previous research that showed antibodies waning after 20 days, but the authors suggest that variations in immunoassay test characteristics and manufacturing may be responsible for the difference.
Increasingly, the scientific evidence seems to suggest


