Researchers at Washington University in St. Louis and the University of Iowa have found out that we don’t just smell with our noses, we also smell with our lungs… sort of. But while your nose might tell you that something is or isn’t good for you, your lungs might make you cough it out.
Smelling with your lungs
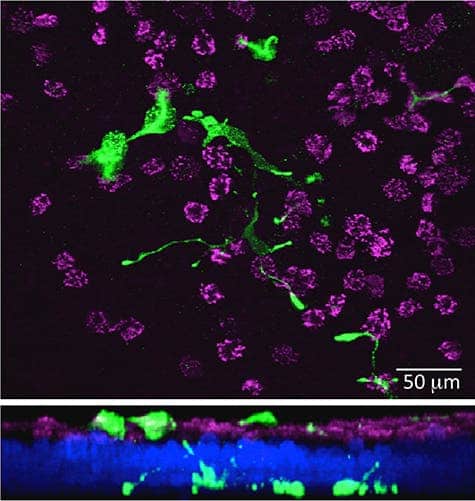
The odor receptors in your lungs are very different from those in your nose. Instead of being located in the membranes of nerve cells, they are located in neuroendocrine cells – cells that receive neuronal input and send out hormones to the blood. So basically, instead of sending out a nerve signal that allows your brain to ‘read’ the smell, they dump hormones that make your airways constrict.
It comes as quite a surprise that an entire class of odor receptors went undetected for so long.
“We forget,” said Yehuda Ben-Shahar, PhD, assistant professor of biology, in Arts & Sciences, and of medicine at Washington University in St. Louis, “that our body plan is a tube within a tube, so our lungs and our gut are open to the external environment. Although they’re inside us, they’re actually part of our external layer. So they constantly suffer environmental insults,” he said, “and it makes sense that we evolved mechanisms to protect ourselves.”
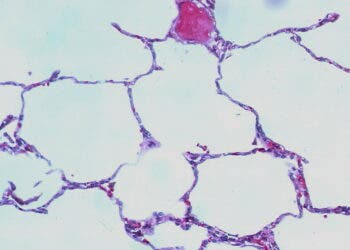
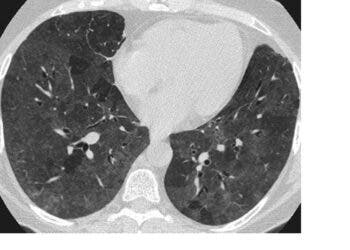
To put it simply, pulmonary neuroendocrine cells, or PNECs are guards, whose job is to make sure nothing harmful enters your lungs. If for any reason, they defect, this could lead to a broad range of afflictions, such as chronic obstructive pulmonary disease (COPD) and asthma. Patients with these diseases are told to avoid traffic fumes, pungent odors, perfumes and similar irritants, which can trigger airway constriction and breathing difficulties.
Every breath you take
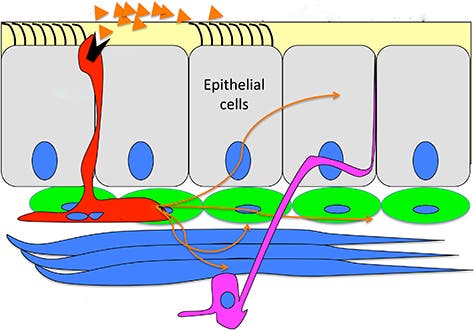
Earlier, a team at the University of Iowa, where Ben-Shahar was a postdoctoral research associate, studied genes expressed by patches of tissue from lung transplant donors. They found a ciliated group of cells that could perceive bitter smells and kick it out, if found dangerous. But people are vulnerable to more than just bitter smells, so Ben-Shahar decided to look again. This time he found that these tissues also express odor receptors, not on ciliated cells but instead on neuroendocrine cells – and this made a lot of sense.
“When people with airway disease have pathological responses to odors, they’re usually pretty fast and violent,” said Ben-Shahar. “Patients suddenly shut down and can’t breathe, and these cells may explain why.”