If it were to become a reality, the gestation of the unborn infant outside of the body (known as ectogenesis), in artificial wombs, could truly shape the evolution of humanity. However, this technology has also sparked fierce ethical-legal debate across the globe. As the prospect of ex-utero gestation draws ever closer, placing social constructs and deciding what is acceptable and desirable in this context has never been more important.
A game changer
Imagine a world where it’s possible to produce children without placing any burden on women — an empowered society where the challenges and health-related risks associated with pregnancy and childbirth have been rendered obsolete. A brave new world devoid of the obstacles to career advancement that women currently face to gestate and give birth to children. Already within the human race’s grasp, the ex-utero frontier would render lifestyle behaviors needed to support a healthy pregnancy obsolete, galvanizing gender equality between every denomination and sexuality.
This state of affairs is what the complete gestation of unborn progeny from conception to term outside of the body, otherwise known as full ectogenesis, could proffer. But, at present, there are many legal restrictions on embryonic research that impede the development of this technology. Meaning, researchers have concentrated on partial ectogenesis comprising artificial wombs which develop the fetus following the transfer from the maternal womb.
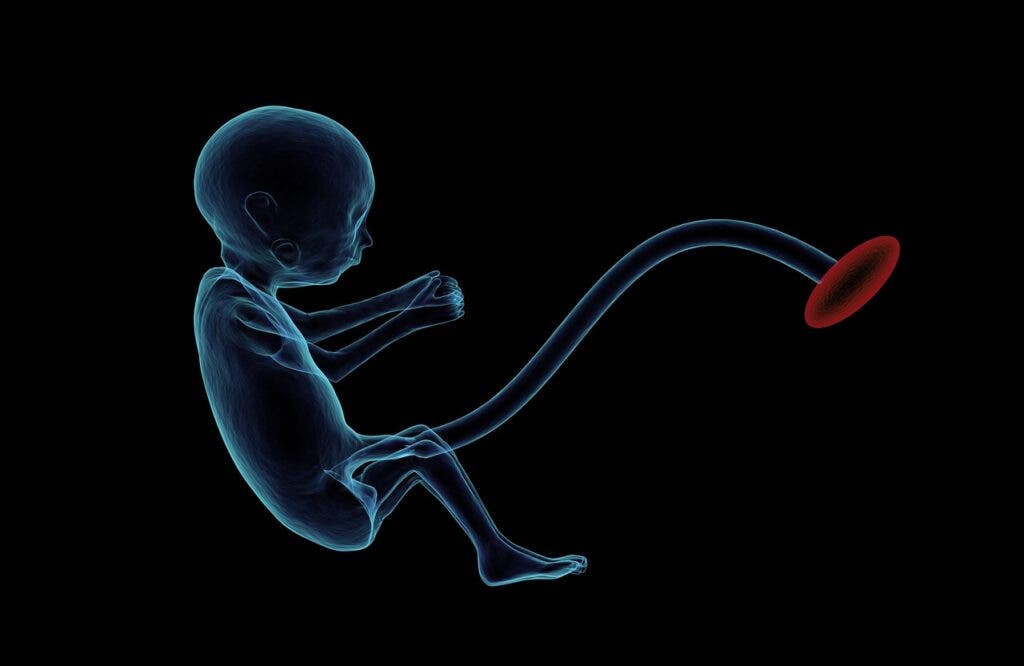
An artificial womb is a device designed to gestate a fetus to term outside of the body. Therefore, the presence of a fetal heart and umbilical cord to support circulation are prerequisites — and once these are met the infant can be transferred from a natural uterus to the artificial uterus, a sort of pre-birth. As over 800,000 babies worldwide are born every year before 28 weeks of age, the main discussion around partial ectogenesis has focused on its potential benefit in increasing the survival rate of extremely premature babies.
Problems begin when a premature baby is transferred to an air-based neonatal unit to support their heart and lung development. This is because exposure to air can lead to many complications as the lungs are not yet fully developed. With partial ectogenesis, premature babies would be transferred to an artificial womb containing synthesized amniotic fluid waiting in the delivery room. Importantly, this ensures that the baby’s lungs remain filled with fluid whilst their umbilical cord is attached to an artificial placenta to improve their organ development, easing the transition to newborn life.
Regarding vital transportation of oxygen and nutrients to the fetus, this takes place via the natural umbilical cord connected to an artificial placenta. Presently, the most common method for the oxygenation and removal of carbon dioxide from a fetus is extracorporeal membrane oxygenation (ECMO), a well-known apparatus for pumping blood and oxygen around the body for long periods. Most recently this technique successfully kept goat fetuses alive for up to 237 hours in amniotic tanks.
Theoretically, an artificial womb would provide the fetus with an environment free of disease, pollutants, alcohol, or drugs sometimes found in the human circulatory system. As a consequence, these desirable conditions may provide fewer hurdles for the infant to gestate to term, hopefully dramatically raising survival rates.
Why there is an urgent need for ectogenesis
Pregnancy is a potentially life-threatening condition where women are at risk of suffering catastrophic injuries or even death during childbirth. Ergo, a solution is desperately needed to avoid injuries sustained during childbirth in developed and underdeveloped economies across the globe. Indeed, even in high-income countries, somewhere between 50–80% of women endure injuries during childbirth. These include anything from muscle tears, lifelong incontinence, holes in organs to breaking the pelvic bones. In fact, the list of ways in which the pelvis and reproductive organs can be damaged during this process is practically endless.
Furthermore, from 1998 to 2009 the rate of severe labor complications increased by 75% during delivery and 114% during postpartum hospital stays according to a 2012 study – these ‘severe complications’ included heart attacks, kidney failure, and aneurysms. To add to these disturbing statistics, according to an interview series from Mother Jones’ Senior editor Kiera Butler, it’s unlikely the medical team will discuss the long-term problems a pregnant woman may face after giving birth — women are often kept in the dark. Butler also found that the majority of women feel that childbirth classes gloss over many hazards, as do many popular pregnancy books with countless doctors refusing to even screen for severe childbirth injuries citing the rarity of the condition.
In general, women find childbirth traumatic as well as invasive leading to post-natal PTSD in many cases. There are also recorded instances where childbirth has induced PTSD connected to past traumas and/or abuse with these women more likely to suffer postnatal depression or psychosis, a condition that can lead to suicide and/or infanticide in the most severe cases. Unfortunately, perinatal depression and/or psychosis can also be experienced during pregnancy due to hormone imbalances. Therefore, research into whether ending the pregnancy earlier to transfer the fetus to an artificial womb could avoid the aforementioned syndromes would be greatly received and provide a possible end to postnatal depression.
As it stands there are also many dangers to the mother and infant in natural gestation. Examples of cases in which prematurely ending a dangerous pregnancy are considered necessary include placental abruption, severe traumatic injury, preeclampsia, chronic hypertension, diabetes, unmanaged uterine infection, significant fetal compromise, maternal cancer, or fetal growth restriction. Combined, these complications in pregnancy are not uncommon, meaning the induced ending or termination of a pregnancy to manage them is also not uncommon.
These chronic conditions during pregnancy can also lead to miscarriages, a factor affecting 15-20 percent of all pregnancies worldwide – consequently, this is where the matter of viability comes in. To explain, the border of viability is the likelihood of keeping premature babies alive – currently standing at 23-24 weeks gestation. As an example, to the UK National Health Service, a baby born dead at 24 weeks is classed as a stillbirth, whereas a deceased baby born at 23 weeks and six days is a miscarriage. This is because anything before 24 weeks is not viewed as viable, i.e. the fetus or embryo is unlikely to survive.
In developed countries with a solid infrastructure, there is a 24% chance of keeping a baby born at 23 weeks alive. But 87% of those who make it will experience complications, such as lung disease, bowel problems, brain damage, and blindness. And although more extremely premature babies are surviving in wealthier countries, the number growing up with chronic conditions has also increased dramatically. Disturbingly, preterm birth is now the greatest cause of death and disability among children under five in the developed world, despite supposed leaps in perinatal care.
How artificial wombs can help
Future developments may allow better prediction of those infants who are destined for extreme premature delivery. Therefore, an option where high-risk pregnancies or live births before 37 weeks could be transferred to an environment where they could carry on gestating would obviously be advantageous.
What can be determined here is that the primary purpose of the artificial womb is to support the gestation and organ development of an infant born prematurely before 37 weeks of age in an artificial liquid-based environment. This is highly preferable as opposed to a neonatal unit where there is still a high rate of morbidity.
Thankfully, the latest incarnation of the artificial womb known as the Philadelphia biobag appears to have sidestepped the complications experienced in neonatal care to successfully gestate fetuses ex utero that have been removed from their mother at 22–24 weeks gestation in human terms.
Ethical considerations start to enter the fray when we consider social end economic disparities. It’s unlikely that pregnant women in communal health systems will be routinely offered ex utero gestation, even when they do have a valid medical reason. Meanwhile, in private facilities where artificial wombs could become a normal part of the reproductive process, causing unnecessary risk to the fetus during transfer to the artificial womb. Although there is no way to predict the severity of injuries during childbirth, women over 35 years of age should automatically present a strong case for partial ectogenesis.
As well as extended infant development, partial ectogenesis could also help enable fetal surgery at an earlier stage of gestation instead of waiting until after birth. Another possibility involves scientists growing human organs in chimeric animal systems to solve organ shortages for people needing transplants. A danger here would be the harvesting of infant organs grown in unregistered artificial wombs in illegal factories. This sad prediction is based on the dreadful current reality that the trafficking of human organs reaps in $1.5 billion a year. Certainly, this is a real concern as trafficked organs now account for 10% of all transplants globally.
A timeline of partial and full ectogenesis
1932-1955: Without a doubt, an honorable mention must go to Aldous Huxley, who first came up with the concept of full ectogenesis and artificial wombs in his dystopian novel “Brave New World” published in 1932. But it wasn’t until the 15th of November 1955 that a patent covering the artificial womb was granted to Dr. Emanuel M. Greenberg who also wrote numerous papers on the subject. Greenberg’s design consisted of a tank filled with amniotic fluid where the theoretical fetus can gestate, and a machine connected to the natural umbilical cord, blood pumps, an artificial kidney, and a water heater. Much of Greenberg’s original design is used as a basis for modern-day systems, with important tweaks.
1996: Many papers were then written on full and partial ectogenesis until 1996 when Juntendo University brought the artificial womb into reality. Their system gestated fourteen goat fetuses that were then placed into artificial amniotic fluid under the same conditions as a mother goat. The team succeeded in keeping the goat fetuses in the system for three weeks.
2002: Fast-forward to 2002, work begins on full ectogenesis. Tissue samples from cultured endometrial cells removed from a human donor are shaped into a natural uterus where human embryos are implanted by Weill Cornell bioengineers. The embryos were correctly implanted into the artificial uterus’ lining and started to grow. However, the experiments were halted after 6 days due to a law preventing human embryos from being kept in artificial wombs longer than 14 days. This rule has been codified in twelve countries.
2016: In line with these rules, researchers at Cambridge University gestated a human embryo outside the body for 13 days using various nutrients to mimic conditions in the womb. The research was only terminated due to the law limiting human embryo research to fourteen days after fertilization. In other words, ethics rather than technology are now the limiting factor.
Circling back to partial ectogenesis, we see (WIRF) in Western Australia begin work on their Ex-Vivo Uterine Environment or EVE therapy in 2013. During an interview with The Guardian in 2020, the research team verified that the lamb fetuses gestated in EVE were between 21 and 23 weeks old in human terms. No one else has ever reported working with fetuses this young, although the team only kept their subjects alive for a week.
2017: Major inroads in partial ectogenesis were made in 2017 with the most viable artificial womb system yet. Researchers at the Children’s Hospital of Philadelphia (CHOP) successfully gestated fetal lambs in a plastic bag filled with synthetic amniotic fluid dubbed ‘the bio-bag’. The bio-bag housed lambs that had been transferred from the ewe’s womb at 110 days, corresponding to 22–24 weeks for humans. The simple design consisted of three main components: a pumpless arteriovenous circuit, a closed sterile fluid environment, and umbilical vascular access.
The vascular access saw the actual umbilical cord of the lambs attached to a machine outside of the bag. It is in this way the artificial placenta provided oxygen and nutrients to the fetuses while removing waste. The premature lambs were then left in their respective bio-bags to develop in a warm dark room to sounds of the mother’s heart. As a result, the lamb fetuses reached all major milestones including the opening of eyes and growth of a wool coat. After which the lambs had matured enough to allow their lungs to fully develop, enabling their ‘birth’ and first breaths of air.
CHOP states their device will have many features that should allow the parent to connect with the fetus going way beyond ultrasound. The planned interactive experience will involve real-time visualization of the fetus within its darkened environment and the ability to play maternal heart and abdominal sounds. Providing an immersive ex-utero reproductive system for both parent and child.
Present-day: The most recent ectogenetic projects include work researchers at Eindhoven University of Technology who’ve been developing an artificial womb since 2016. Their artificial womb and placenta aim to provide a natural environment for the baby to ease the transition to newborn life. In 2019 this consortium was granted a subsidy of 3 million euros, with a second grant of 10 million euros currently in progress.
Work relating to full ectogenesis is still ongoing with two papers recently published in the Nature journal. The studies report the out-of-body generation of human blastocysts, the crucial stage the human embryo reaches approximately five to six days after fertilization right before it implants into the uterus. This was achieved by differentiating non-embryonic cells into blastoids or blastocyst-like cells. In one study, scientists treated stem cells with specific growth factors to generate the blastoids. In a second study, adult skin cells were reprogrammed into blastoids.
Researchers at the Weizmann Institute of Science have also reportedly gestated mouse embryos ex-utero into fetuses with fully formed organs. They achieved this by implanting mouse blastocysts into an artificial placenta that contained special media and gases to study organ development. The resultant mouse embryos were healthy until day 11 before dying, maintaining viable gestation for about halfway through the animals’ normal 20-day gestation. These results have led many specialists to believe that it’s only a matter of time before this technology generates healthy newborn pups.
To surmise, what these studies are telling us is that trials in full ectogenesis are extending the time embryos can survive to develop outside of the body, and the transfer and development of fetuses in artificial wombs are pushing back the window of viability for the survival of premature infants. Expect these two crucial points to meet within the next two decades.
What are the disadvantages of an artificial womb?
There is much contention around the socio-ethical connotations of partial ectogenesis. What has already been posited is that based on the timeline of pre-existing reproductive technologies, it is likely to be expensive and restricted to highly equipped neonatal intensive care units.
Certainly, at the inception of this science global disparities in health outcomes for pregnant people and infants are in danger of being increased, as is racial inequality within the wealthiest nations. For instance, 94 percent of all maternal deaths occur in low and lower-middle-income countries according to the WHO. So is it realistic to expect prospective parents in these regions to be offered partial ectogenesis?
The answer to the preceding question is a resounding ‘no’ – surely this technology would mean universal coverage for reproductive, maternal, and newborn healthcare will finally be addressed. For this reason, equal care for all should be fundamental to the development of partial ectogenesis. Particularly in those regions suffering high maternal death rates and/or race-based discrepancies.
Another important disadvantage is that a fetus would not have the advantage of antibodies transferred from its mother until it started breastfeeding. Also, vaginal flora likely contributes to the health of an infant. However, this is the same state of affairs for cesarean section and perhaps a necessary exchange where a pregnancy has been deemed dangerous. There could also be other issues related to nutrition, pulsatile blood flow, and hormones regulated by the native placenta that may be impossible to simulate in an artificial environment. Moreover, there are concerns from the scientific community that children who develop in an artificial womb may lack some essential bond with their mothers that other children have. This could be counteracted by the use of immersive tools CHOP is now designing for its system. Offering an even stronger bond between both parents and the infant dependent on this technology evolving.
In Aldous Huxley’s vision, we see a dystopian society that engineered ex utero humans in massive reproductive factories. It’s highly feasible this could well become a reality as blastoids are already being generated in transparent vessels. Comparably, the use of artificial wombs could give rise to engineered humans that nobody feels any responsibility toward whilst watching the product of genetic editing in real-time. There is a danger these made-to-order embryos could be the initiation of baby factories for expensive adoptive transactions.
As renowned philosopher Professor Julien Murphy notes, women who are smokers, drug users, or casual drinkers and do not wish to alter their behavior could also benefit from ectogenesis. However, the author feels this throws up questions as to how parents with addictions will handle child-rearing once the child is born. Yes, this is a deconstructed egalitarianism where both parents are free to live a hedonistic, self-abusive lifestyle whilst their child is gestating. But how can this be viewed as an advantage where the child is endangered by the very same parental behaviors once they emerge from the artificial device? Will their parents suddenly give up their substance abuse once their child is delivered into their arms?
Further, should prospective parents living unhealthy lifestyles be asked to sign legal documents which require them to give up their children once they are removed from their bodies and transferred to artificial wombs? And what would constitute an ‘unhealthy lifestyle’ as we become more health aware as a society? Could we see serious breaches of human rights here with children becoming a ward of the state due to overreaching health scales and regulations that parents-to-be must follow? Due to the current state of childcare services worldwide, will this even be possible to police? It goes without saying that childcare services and police protective services for children need to be overhauled and improved before this technology arrives in our hospitals.
How the artificial womb could usher in a new age of gender equality
There are many positive premises regarding the artificial womb and gender parity with most experts in agreement that this eventuality could herald the era of true equality between all sexual denominations. Crucial to this, ectogenesis is also defended because it would promote equality among fertile, infertile, lesbian, and transgender women.
Firstly, women’s central role in producing children condemns them to a less competitive place in the labor market, fewer career advancements, less remuneration, and difficulty accessing certain professions.
So there can be no doubt that both partial and full ectogenesis will promote full equality between male and female workers. Still, how will employers view the natural full-term gestation of a fetus where partial ectogenesis is an available option?
The second point focuses on ectogenesis enabling women to have children who are unable to reproduce for social or biological reasons. Primarily, the production of a genetically related child for infertile women, and fertile or infertile men, would rely on the development of full ectogenesis. All the same, even where partial ectogenesis gives rise to unrelated offspring this would greatly equalize reproductive capacities in nonbinary groups. Indeed, even single men or gay men could become parents without the need of a female partner, overseeing and coordinating the immersive gestation experience of their offspring to term themselves.
What’s more, this socio-politico perspective allows for the elimination of several life-changing risks and burdens associated with pregnancy and childbirth — as well as some of the unfair distribution of childrearing responsibilities between men and women. Ectogenesis also promises to make the metamorphosis of the transgender female replete. In a possible devolution of the feminist principle, transgender women will be given the choice of settling into their traditional role of motherhood and keeping house. A step back to leap forward it would seem.
Another reality the artificial womb may bring about is the inception of the ex-utero ‘fourth trimester‘ where infants are gestated for 12 months instead of just nine. Already dreaded by many new parents around the globe, the fourth trimester is the period where a newborn baby is in a sensory overload of sights, sounds, and smells. As well as a frequently colder environment where they’re not constantly supported by the protective amniotic fluid.
This notoriously difficult period after birth could be ended by an artificial womb lengthening the gestation and development of the fetus to a year – providing a far more robust baby and fewer sleepless nights for parents. The end of the traditional fourth trimester could also make it easier to share childcare uniformly between parents as a 3-month-old ‘newborn’ could make this job a lot less stressful. Importantly it could also aid in the treatment of infants set to be born with defects or ailments. Here the luxury of an extended gestation could afford a greater chance of recovery from surgery or drug regimes administered in a transparent artificial womb.
Finally, full ectogenesis could also end the practice of surrogacy and its related legal complications and navigated relationships with the pregnant individual. For some prospective parents, an alternative to surrogacy gifting more control over the process of gestation may prove preferable. To stress, this may not work so well with partial ectogenesis denoting the transfer of the fetus from the uterus of the surrogate at an early stage of pregnancy. Could this even be justified?
The moral and philosophical implications of the artificial womb?
The development of the artificial womb raises a multitude of bioethical and legal considerations along with serious implications for the ongoing abortion debate. Owing to the fact partial ectogenesis could expand the range of fetal viability, questions have been raised as to the possible role it will play within abortion law. As a consequence, the legal definition of the termination of pregnancy may be redefined once the fetus is transferred from the host to an artificial womb.
The transference debate may also cause further problems as the fetal window of viability increases with improved technology – where the border moves from 24- down to 19 weeks, for instance. This increased window of viability, where the fetus can be transferred to an artificial womb at an earlier stage of development than the latest stage allowed for the termination of pregnancy, may also be deemed criminal depending on the abortion laws in the region. This increased window of viability in all likelihood will change abortion law, protecting the embryo and fetus at an even earlier stage of pregnancy.
In that event, women could be required to provide legal justification for their decision to opt for artificial gestation. Examples may include a dangerous pregnancy or severe injury risk during childbirth – although it is unlikely that the fetal transference would be legally sound based on a short-term health risk to a woman. Possibly meaning any long-term risks must be proven before the pregnancy is terminated and the fetus transferred to the artificial womb; this will not be an easy task.
Another ethical dilemma posed by the ectogenetic future is a case scenario where fetuses aborted by mothers are then rescued and adopted. In that reality, some women might seek out dangerous backstreet abortions rather than using a legal transference to give their child up for adoption. It’s no wonder that whether artificial wombs should be allowed to influence the pro-choice movement is already under debate with ex-utero gestation and its product already set to become a matter for criminal law.
Ectogenesis may also heighten economic inequality – where wealthy prospective parents may opt to pay for artificial wombs – while the less financially secure will rely on women to gestate their babies. Existing disparities in nutrition and exposure to pathogens between pregnancies across socio-economic divides may also be intensified – raising the issue of distribution of access. For instance, will artificial wombs receive government funding? If it does, how should the subsidies be distributed? Once again, will there be a threshold or health regulations the parent or parents must meet?
The potential for serious human rights breaches is once again regurgitated from the mouth of this purported liberating technology.
Conclusion
To conclude, full ectogenesis will likely not exist for decades, but artificial wombs (and partial ectogenesis) are coming up fast. We need to ensure that, when they do arrive, we’re ready — and society values women for more than just their reproductive capacity. Moreover, authorities should ensure that this technology benefits people who can’t get pregnant for biological rather than psycho-addictive reasons.
According to Manchester University, partial ectogenesis may be ready for human testing in the next 5-10 years. In that event, it is vital to consider its implications in advance of its development – this means broader social and policy considerations are needed for their use in non-emergency situations. Common sense dictates that it will be easier to defend using artificial wombs in emergencies, such as saving the lives of premature fetuses or, one would hope, the person who is pregnant.
For example, documented evidence indicates women from minority groups are at a much higher risk of experiencing serious complications or fatalities during gestation and childbirth. This technology could greatly improve survival rates in these ecological niches, helping to close health disparities, providing social emancipation. To enable this, it is essential that ectogenesis is distributed evenly amongst people from disadvantaged backgrounds and/or those with disabilities.
Now, studies on full ectogenesis are pushing forward the time in which ova can be grown into embryos and sustained in vitro – while research into non-humans gestating in artificial wombs is pushing back the window of viability for premature fetuses. Thus, as we get better at extending the lives of embryos outside the womb, and keeping ever more premature babies alive, there will come a time when those two points meet and full ectogenesis is born. It is therefore imperative to collate and ramp up the discussion around this burgeoning field of science. This is because the obstacles will be legal and ethical, not technological.
While this may sound futuristic, many technologies that seemed revolutionary a few years ago are now pretty common. Look at IVF – it was once dystopian science fiction, then an ethical minefield, and then the cutting edge of assisted reproduction – now, IVF is a normal part of reproductive treatment.
So once bags and tubes can replace a womb, pregnancy and birth can be redefined. In that, if gestation no longer has to take place inside a woman’s body – it will no longer be female. This beautiful event will change the meaning of motherhood as genders blur into one, severing our confinement within a set definition. This will be a massive socio-ecological phenomenon, changing the world irrevocably. It’s up to us to decide if it is for the better or worse.


