In rural Romania, in a small town called Sadova, some 200 km west of the country’s capital Bucharest, the local community is trying to ensure that their daughters don’t have to pass through the dread of cervical cancer.

Sadova is an unlikely success story in what is an otherwise struggling vaccination campaign — an oasis of vaccination in a region where vaccine hesitancy is taking firm root. Out of 66 teenage girls registered at the local medical practice, 60 have taken the anti-HPV vaccine: a huge percentage, considering that only around 1% of Romanian teenage girls are being vaccinated.
At the core of this local success story is doctor Gindrovel Dumitra, who has managed to earn the trust of his patients.
“We trust our doctor, we’ve followed his recommendations every time,” says one of Dumitra’s patients, who has a 13-year-old daughter vaccinated anti-HPV. “We know that the vaccine offers protection against cervical cancer,” she tells me at the doctor’s office.
Of course, like any mother, she was concerned; she wanted to ensure there would be no side effects or problems caused by the vaccine.
“I was indeed afraid,” the mother says. “But after the first discussion [with Dumitra], my fears vanished. My daughter wasn’t afraid at all,” she adds.
In Romania, as in the rest of the world, trust is an integral part of any successful vaccination campaign, and people are more inclined to trust their doctor than politicians or other authorities, Dumitra says. But it’s a long process. In Dumitra’s clinic, patients come in for various different health problems, but they also come for another reason: they’re looking for his advice.
“We’re still in the stage where we’re re-earning people’s trust,” the doctor says. “A lot of parents are still searching for an infusion of trust. This is the reason why we talk closely to mothers [about HPV vaccination], even when they come for other problems.”
Whenever a parent comes by his practice, he always tries to drop in a word or two about HPV vaccination. The approach that seems to work best is to explain the benefits of vaccinations in simple, to-the-point terms. Usually, cervical cancer is not a visible problem in the community so sometimes, the doctor tries to mention problems that may be more relatable, like genital lesions.
While the problem may not be that visible, it takes a major toll. Globally, an estimated 604,237 women were diagnosed with cervical cancer in 2020, and this is the most common cancer among young women in several parts of the world — including Romania. In 2020, 1,805 lives were lost to cervical cancer in Romania. These are all preventable tragedies, says Dumitra.
“Every year, we lose over 1,700 women. We’re talking about women aged 25-65, young women who are mothers, who have children, who are leaving a family behind,” the doctor says.
Cervical cancer is one of the few types of cancer that can be directly prevented. In over 90% of all cases, it is caused by HPV — the Human Papillomavirus, which has several high-risk cancerous strains, and several strains that cause warts. The virus is almost ubiquitous. The odds that an unvaccinated woman acquires this virus is around 85%, and most infections happen at early ages, between 15 and 23 years old, through sexual contact.
The good news is there are several safe and effective vaccines that can protect against this virus, and consequently, against this type of cancer. But a vaccine can only help you if you take it.
The vaccine works and is safe but myths persist
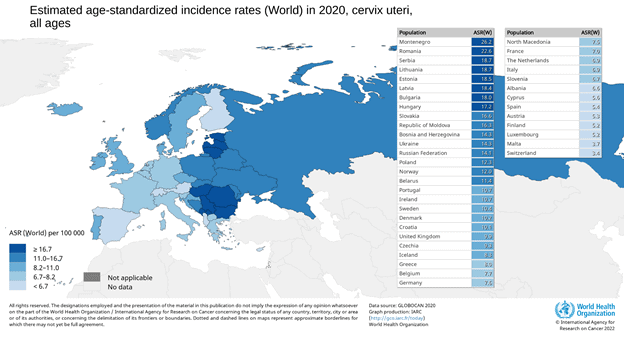
Romania has the highest cervical cancer incidence and mortality rate in Europe, with up to 17 in 100,000 women killed by the disease, over four times the EU average; to make matters even worse, the cervical cancer screening rate in Romania is also one of the lowest on the continent. While other countries like Australia and the UK are well on their way to eradicating cervical cancer, Romania is taking wobbly steps towards a proper HPV vaccination campaign.
“Indeed, uptake and acceptance in the Eastern European countries is not always at the high rates we would hope for, and this is of concern, particularly because the region does have relatively high cervical cancer incidence,” says Paul Bloem, Technical Officer in the Immunization, Vaccines and Biologicals Department at the World Health Organization. “There are many factors at play, not all of them particularly related to HPV vaccines.”
Romania started its first HPV vaccination campaign in 2008 — one of the first countries to do so. But the campaign was a fiasco. Just 2% of Romania’s teenage girls got vaccinated, and the campaign was dropped. Back then, concerns about potential vaccine side effects and that the vaccine could somehow push girls to start their sex life earlier dominated the national discourse, and authorities were inefficient at pushing back against these myths. Now, we have more than a decade of additional data saying the HPV vaccines are safe and effective but myths persist.
In fact, over the COVID-19 pandemic, “vaccine hesitancy has normalized” and has become a “reasonable position” in Romania, says Simona-Nicoleta Vulpe, a PhD candidate in Sociology at the University of Bucharest.
“The decision to get the vaccine depends a lot on trust,” Vulpe says. “People get vaccinated when they trust one or more entities that encourage vaccination — whether it’s doctors, experts, public authorities, media, or just people they know,” the sociologist adds.

Trust and empathy are also crucial tools for gynecologist Alina Diaconu, from the Renașterea Foundation in Bucharest. Diaconu has participated in several pap screening campaigns and also recommends vaccination to her patients, and she also says there’s a lot of disruptive noise coming from the public sphere.
“During a consultation, it takes a lot of time to just take away the baggage of information coming from social media, Google, and other similar sources, and only after that I can tell the patient what’s going on and actually start the consultation,” the doctor says.
Although HPV vaccines have been shown to prevent around 90% of cervical cancers (as well as 90% of anal cancers, 70% of oropharyngeal cancers, and 60% of penile cancers), the success of a vaccination campaign hinges on the ability of authorities and doctors to communicate these benefits against baseless concerns. We’ve clearly seen how much public doubt can weigh on a vaccination campaign, not just in the 2008 HPV one, but also in the COVID-19 pandemic: in Romania, less than half the population is COVID vaccinated, despite wide availability. As Dumitra emphasizes, trust is an “essential element” of any vaccination campaign, and trust requires empathy, expertise, and time.
But trust alone can’t build a vaccination campaign.
Can Romania’s new vaccination campaign succeed?
Romania’s 2008 vaccination campaign failed due to a lack of money as well as inefficient communication. But this time around, there are some encouraging signs.
After distributing 40,000 doses in 2021, the Ministry of Health has expanded the campaign to 195,000 doses, for which there is already a demand. Officials are also investigating the possibility of vaccinating boys, with an assessment and decision “will be coming,” the ministry says.
But the doses coming into the country will be enough to vaccinate under 100,000 people. For a country with over one million teenage girls, this is hardly enough.
Because of insufficient doses, HPV vaccination was mostly restricted to well-off families that could afford to buy the vaccine themselves. The price of a dose is now over 120 EUR — girls under 15 need two doses, while girls over 15 need three doses.
Government stocks have been insufficient and unreliable, says Ana Măiță, the head of an NGO called Mame pentru Mame [Mothers for mothers] which focuses on the health of women and mothers. Currently, parents wanting to vaccinate their girls first need to fill out a form and send them to their doctor. These forms are centralized and ordered based on their submission date, and every three months, the doctor asks the Ministry for the required doses. It’s a cumbersome and inefficient process, Măiță says, especially problematic for vulnerable families.
“Romania doesn’t have an anti-HPV vaccination program,” Măiță says. “Romania has a sort of à la carte menu for the few parents that understand the importance of HPV vaccination. I’m fighting so we have a true vaccination program, but Romanian officials haven’t yet set any clear goals like the EU recommends.”
“I often come across situations where parents want the vaccine but don’t have access to it,” she adds.
The goals set by the EU are those recommended by the World Health Organization (WHO): vaccinating 90% of all adolescent girls by 2030 and organizing screening programs to include 70% of women of all ages. Romanian officials have stopped short of accepting these figures as clear targets, but they say they’re working on it.
“The Ministry is considering implementing a sustainable vaccination program against HPV, aligned with the goals set out in the Europe Beating Cancer Plan, which includes vaccination of 90% of the target population of teenage girls,” one official explained.

Ironically, the biggest roadblock for the campaign is money – it’s ironic because Romania, like every other country, has every financial reason to invest in this type of prevention. According to studies, for every dollar invested in anti-HPV vaccination, a country saves $20-$50 in the long term; immunized people tend to be healthier, are at lower risk of hospitalization for HPV-associated problems, live longer, and are active in the workforce longer. Basically, countries can save a lot of money while also offering girls and women a better, healthier life.
Unfortunately, many countries invest too little in preventing diseases — and this is exactly the case in Romania. Romanian authorities haven’t purchased enough doses and haven’t invested nearly enough to bring HPV vaccination into the public eye of the general population. Even the country’s National Cancer Plan foregoes prevention, focusing instead on therapy and treatments. Unsurprisingly, this also means that most people are unaware of cancer prevention methods such as HPV vaccination.
According to a regional GfK study carried out in 2016, two out of three women in Romania haven’t even heard of the HPV infection, and 1 in 10 women have not attended any screening in the past ten years. Just one in four women have had a pap smear in the past three years.
Romania needs a “paradigm change regarding women’s health,” says endocrinologist and former Health Minister Ioana Mihăilă, who was one of the pioneers of the country’s new HPV vaccination campaign. It was during Mihăilă’s term that free vaccination was extended to girls aged 18.
“Anti-HPV vaccination is the best method to prevent cervical cancer, which is why we’ve extended the age group so that more at-risk people can receive a free vaccine,” Mihăilă said in September 2021, announcing the move.
Mihăilă, like all doctors we’ve interviewed, also wants boys to eventually be vaccinated. Although girls are most at risk from HPV, boys can also suffer from some HPV-caused cancers and can spread the virus. At the moment, Romanian parents who want to vaccinate their teenage boys have only one choice: buying the expensive vaccine (assuming they can even find it in stock).
Common problems
Romania’s setbacks are shared by many other countries. While in countries like the UK and Australia, vaccination campaigns have been successful and have led to plummeting cervical cancer rates, others haven’t been as successful. Denmark, Ireland, the USA, and Japan are just some of the countries that have had unsuccessful campaigns in the past.
Part of this can be traced back to insufficient communication efforts.
“With hindsight, one can also say that vaccination programs often underestimated that this vaccine – given the target of girls of this age – needs much more and sustained communication and sensitization efforts over several years to be accepted by the population. The normal, tested ways of introducing childhood vaccines may have been insufficient,” Bloem notes. In this day and age, no vaccination campaign can succeed without an adequate communication campaign behind it.
“Efforts have to be based on the latest communication insights, using a plethora of channels to reach people where they are, including digital media, and need to target girls and parents as well as health workers, teachers, and other community stakeholders,” Bloem notes.
The good news for countries looking to kickstart anti-HPV vaccination and prevent cervical cancer is that they can draw inspiration from countries that have had success.
“We are very pleased that the positive impact of the HPV vaccine programme in the UK is now being seen. This year, a study we funded in England showed the vaccine dramatically reduced cervical cancer rates by almost 90% in women in their 20s who were offered it at age 12 to 13,” said Alexander Wright, Global Lead at Cancer Research UK.
There are actually not many differences between the strategies deployed in developed and developing countries, the WHO official explains. The main difference is that higher-income countries tend to have more schools that can play a role in such programs but tend to have more vaccine hesitancy, whereas, in lower-income countries, vaccination is more often well-received, although developing countries may find it challenging to support the costs of a national campaign.
Mihăilă also believes that drawing lessons from other countries are a key element, especially when it comes to making long-term plans. Of course, any plan must be tailored to the local cultural and logistical challenges, but some things are universal: one of these things, the former minister says, is the courage to take on such campaigns even if they may be unpopular with some parts of society. Even in the strong vaccine hesitancy context currently shaping up in Romania, taking on HPV vaccination has never been more important.
“I think we’ve lacked the courage,” Mihăilă says. “It takes political courage to take on preventive health policies, but these are the most impactful and sustainable policies in the mid and long-term. We have to take them on, even if it means challenging the disinformation channels.”
A roadmap for eradicating cervical cancer
Romania, like many other countries, has wasted over a decade in which it could have tackled cervical cancer. But things may be looking up. Dumitra, the architect of one of the early HPV vaccination success stories in Romania, says that even though the previous campaign failed, he now sees some steps being taken in the right direction, and a window of opportunity may be opening up.
“We’re on an upward trend when it comes to parents accepting the HPV campaign,” the doctor says.
Although cervical cancer is typically caused by the types of high-risk HPV strains, vaccination also protects against genital warts, which are typically caused by low-risk HPV strains.
“Most patients know someone who had a wart and had to cauterize it or do some form of treatment,” says Dumitra. Relating with parents is essential, and this includes considering the concerns expressed by patients, the doctor notes.
The vaccine works best if it is administered before commencing sexual activity. In Romania, this translates to an average of 17 years for boys and 18 years for girls. While people in their 20s and beyond are also likely to benefit from vaccination (Australia recommends the vaccine for females aged 9–45 and males aged 9–26), the priority should be focusing on the early teens.
“The best age to vaccinate girls is 11-13, but the vaccine is still very effective at preventing infection at older ages,” says Peter Sasieni, Professor of Cancer Prevention at King’s College London and co-author of a study analyzing the success of HPV vaccination in the UK. “There are two issues with vaccinating older teenagers in many countries. One is that the highest uptake rates have been seen in school-based programmes and as people age it is much harder to achieve very high population coverage. The other is that many 18-year-olds will have already been infected with HPV before being offered the vaccine, and once infected (with a particular HPV type) the vaccine offers little or no protection against persistent infection or progression to cancer. Hence, whilst individuals in their late teens and 20s may benefit from HPV vaccination, I do not see it as a public health priority.”
The UK’s strategy, well documented by now, shows a roadmap that can be implemented in other places as well. The country introduced vaccination in 2008 for girls aged 11-13, and then extended it up to girls aged 18. Then, they moved on to boys aged 11-13, and females up to 25 years old — a strategy that Romania may also be moving towards.
This can be done step by step and patient by patient, Dumitra believes. But it won’t be easy. From political challenges to financing and disinformation, the logistics of the vaccination campaign are bound to be difficult. But the results will be worth it. As we’ve clearly seen already, we have a vaccine that could essentially eradicate a type of cancer — an achievement well worth the effort.
“HPV vaccination campaigns are critical for the elimination of cervical cancer as a public health problem,” Sasieni concludes. “If we could vaccinate 90% of girls globally by the age of 15, we would be well on the way to ensuring that cervical cancer becomes a rare disease in future generations.”
This article was funded by the European School of Oncology through its Cancer Journalist Grant scheme.