In the seemingly endless March of 2020, it almost looked like the pandemic would never end. A one-year waiting period for a vaccine was considered very optimistic, and there were no guarantees. But the vaccines came faster than expected and we’re on target for an unprecedented immunization campaign.
Countries all around the world are starting to eye the end of the pandemic — or at least some return to a degree of normalcy. In order for that to happen, we need to reach some form of herd immunity or at least get very close to it.
So how much of the population do we need to vaccinate to reach herd immunity? Estimates fall somewhere between 60% and 90%. No one really knows for sure, but here’s what we do know — and why all this does matter.
What’s herd immunity anyway?
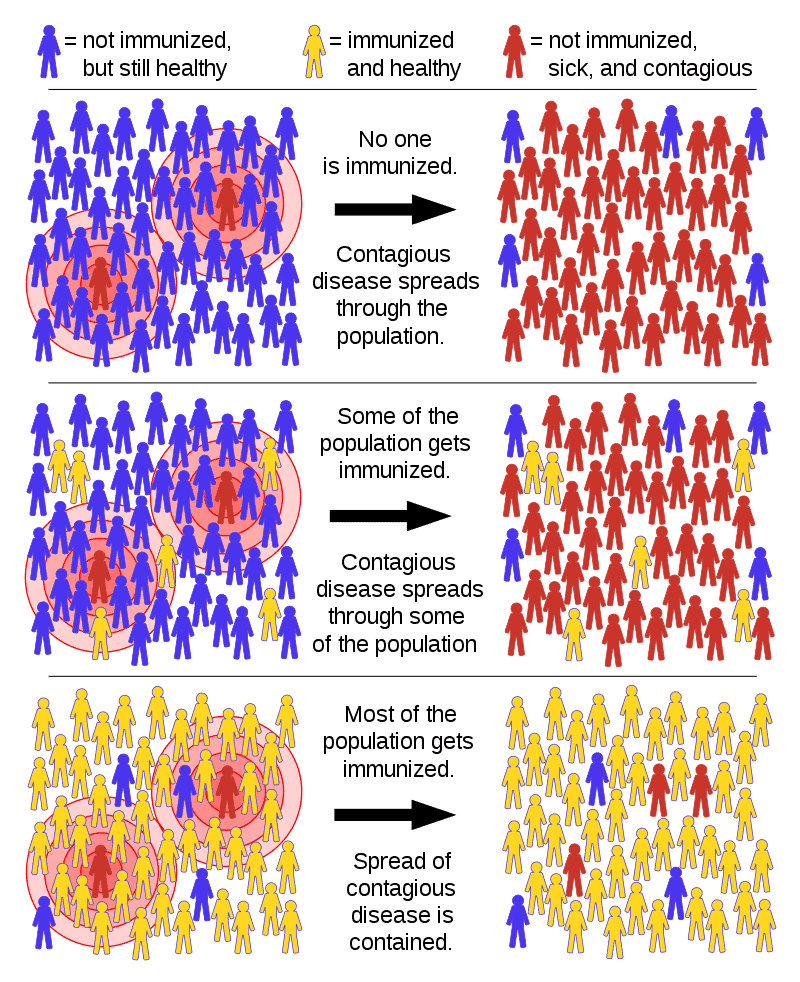
Herd immunity isn’t a novel concept — we’ve dealt with it long before the COVID-19 pandemic. Herd immunity happens when enough people are immunized that the spread of infection throughout the community as a whole is no longer possible. When herd immunity is achieved, people within the community are protected — even those who don’t have protection themselves.
It’s essentially a way of protecting everyone in the society, including those who can’t develop immunity for some reason or can’t be vaccinated due to medical reasons (immunocompromised people, for instance).
Herd immunity is reached when a large enough portion of the population becomes immune and the virus can’t find routes of transmission anymore. That’s a way of saying we’re keeping the virus under control and it won’t be a major part of our lives anymore.
Herd immunity can be reached through vaccination (the easy way) or by getting the disease (the hard way). The first one is definitely better than the second. For some diseases that mutate often (like the flu) and can reinfect you, herd immunity is never achievable through infection alone — and for the coronavirus, that’s also not an option.
Herd immunity — but only through vaccination
In the early days of the pandemic, herd immunity seemed like a good idea… to some. Despite being popularized by politicians such as Donald Trump and Brazil’s Jair Bolsonaro, however, the idea of reaching ‘herd immunity’ through exposing people to the virus is unethical and, at best, scientifically questionable. It would be somewhere between very risky and catastrophic.
We’re already seeing it happen: in the Brazilian city of Manaus, 76% of the population had been infected with SARS-CoV-2 by October, 2020. Yet in January 2021, a new surge of hospitalizations was reported in Manaus, with one dangerous viral mutation emerging in the process. Whether it’s due to antibodies waning, a new mutation, or some other explanation, it’s a case study that clearly shows allowing the virus to run free isn’t a solution.
Most researchers also agree that letting the virus “run its course” through the population is a recipe for disaster. It won’t just end up killing and hurting a lot of people, but at the end of the day, it could still end up being for nothing because we don’t know how long immunity lasts.
There are plenty of unknowns when it comes to natural immunity, but let’s say, for the sake of the argument, that immunity would last an average of 12 months. If immunity were to wane after one year, we’d have to start all over again after one year and we wouldn’t have achieved all that much. With a vaccine, however, that would be a much different situation as we could repeat vaccines yearly.
It’s not just theory — this is pretty much what we’re doing with the flu viruses. We’re very, very far from achieving herd immunity for the flu, but plenty of people are immunizing with a vaccine every year, and it’s working.
Presumably, we will need to do the same thing for COVID-19 for a while. While some countries may reach herd immunity as early as 2021, it’s unlikely that the entire planet can reach it, which means that the virus will still run amok in some parts of the world, and will have a chance to mutate and change (which means we would need to change vaccines and have new injections every year or so).

How many people need to be vaccinated for COVID-19 for things to get back to normal?
Until now, we’ve spoken in general terms, but let’s zoom in on COVID-19. How many people do we need to vaccinate to achieve herd immunity for COVID-19?
The percentage of people who should be immune in order to achieve herd immunity varies with each disease, particularly based on how contagious the disease is. For measles, the herd immunity threshold requires about 95% of the population to be vaccinated. For polio, it’s 80%. For the flu, some estimates put it at as low as 44%. For COVID-19… we’re not really sure.
| Disease | Transmission | Herd Immunity Threshold |
|---|---|---|
| Measles | Airborne | 92–95% |
| Pertussis | Airborne droplet | 92–94% |
| Diphtheria | Saliva | 83–86% |
| Rubella | Airborne droplet | 83–86% |
| Smallpox | Airborne droplet | 80–86% |
| Polio | Fecal-oral route | 80–86% |
| Mumps | Airborne droplet | 75–86% |
| SARS | Airborne droplet | 50–80% |
| Ebola | Bodily fluids | 33–60% |
| Influenza | Airborne droplet | 33–44% |
The initial estimates put a tentative herd immunity threshold at 67%, with a reproduction number of 3 (every person that gets the virus would pass it to 3 others in a population where all individuals are susceptible to infection). We’re still not sure what the reproduction number is, but for the first part of the pandemic, the 60-70% was largely circulated by researchers.
However, although that range is still cited by the World Health Organization and still quoted, US officials have begun quietly moving the figure upwards. Anthony Fauci started saying “70, 75 percent” in television interviews and, in an interview with CNBC News, he said “75, 80, 85 percent” and “75 to 80-plus percent.” Quoted by the NY Times, Fauci would “bet his house” that COVID-19 isn’t as contagious as measles, and he believes the figure needed for herd immunity isn’t as high as 90%. But it’s probably also a bit higher than 70%. We also need to account for the fact that some vaccines seem to perform somewhat worse than the others, and in this case, the effect would need to be counterbalanced by a higher vaccination rate.
Simply put, the herd immunity threshold for COVID-19 seems to be around 70-80%, but we’re not entirely sure where it lies.
Mutations: another incentive for quick vaccination
We don’t necessarily need herd immunity to get things back to normal. The more people we vaccinate, the more people become immune, and the more the risk is reduced. Herd immunity guarantees we protect a vulnerable part of the population, but there’s another advantage to it: it reduces the risk of mutation.
Viruses change and mutate all the time — some faster, some slower. For the most part, these mutations don’t really amount to much. But every once in a while, a dangerous mutation does arise — a mutation that can make the virus more contagious, more dangerous, or more resilient to vaccines. The idea of vaccinating a big chunk of the population only for the virus to mutate and evade the vaccine is one of the worst possible scenarios. This is why vaccination isn’t really a national race: viruses don’t really have borders. If some nations reach herd immunity and others don’t, mutations can still arise and threaten the vaccinated nation.
Viruses can’t mutate if they can’t replicate. The more people we vaccinate, the closer we get not only to herd immunity but to truly ending the pandemic.
Are we there yet?
We’re not even close to herd immunity at this point, but it’s quite plausible that by the end of this year, several countries can achieve it. If we want to vaccinate 80% of the population within a year, we need to vaccinate 6.6% of the population every month. In the US, for instance, that means vaccinating 21 million a month.
Despite a rough start, it can be done. Assuming that vaccine hesitancy doesn’t start taking a toll (recent polls show it’s plummeting), our main obstacles are production and distribution chains. We already have several working, approved, safe vaccines. Production is scaling, the logistics are already being deployed, we could get there.
However, disparities (both national and international) are likely to plague vaccination campaigns. The dangers of vaccine nationalism are very present and scrambling to be the first to inoculate your population will achieve little if others go unvaccinated as a result. The pandemic doesn’t affect everyone equally, but it does affect everyone — and only together can we truly overcome it.


