Most diseases are caused by pathogens attacking our bodies. A small part of them, however, are caused by our body attacking itself. They’re known as autoimmune diseases, and lupus is one of them.
Its exact symptoms vary from person to person and from time to time, but the most common include fatigue, confusion, memory difficulties, a distinctive ‘butterfly’ rash, as well as stiffness, swelling, and pain in the joints.
Nobody likes being sick. We’d all rather take a pill or some gulps of syrup than let some yucky bacteria or viruses keep running roughshod through our bodies. But what if you get sick but there’s no pathogen to wipe away? Can a disease be caused not by any external source — but by your own body?
Sadly, yes. One class of such diseases, known as autoimmune conditions, are produced by our own immune systems attacking our healthy tissues. Sometimes, a bit confusingly, they can also be produced by an immune system that’s too tame and doesn’t act as it should. Regardless, one of the most well-known and arguably most representative diseases for the autoimmune family is lupus, clinically known as systemic lupus erythematosus, SLE. It can also, but not necessarily, produce a wide range of the symptoms seen in other autoimmune diseases, so it’s also quite educational.
So let’s take a look at what we know about SLE, its causes, what symptoms to look for, and what treatments are available.
Homo homini lupus
That’s one of my favorite proverbs, “man is a wolf to man”. It’s meant to warn you that people will often be cruel to others in pursuit of their own interests, but if you take it quite literally, it’s actually a pretty good description of SLE. Still, the idiom and the name aren’t related. To the best of our knowledge, the disease was named sometime during the 13th century by Rogerius, a physician, as the skin rashes it can cause reminded him of a wolf’s bite. Which, if you ignore the whole ‘disease’ part, is pretty cool.
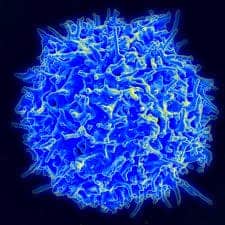
But let’s get back on track. Lupus is a disease in which certain antibodies — known as autoantibodies — target an individual’s own proteins, much like typical antibodies do with viruses. In effect, this makes the patient’s own cells and tissues the target of their own immune system. There are a lot of different tissues throughout your body, and each of them is made up of a wide range of proteins. As such, the symptoms that lupus can cause are similarly varied.
The most common ones include painful, swollen joints, fevers, mouth ulcers (for seemingly no reason), red skin rashes in distinctive shapes (typically from light exposure), swollen lymph nodes, fatigue, memory issues, chest pain, hair loss.
Symptoms can also include dry eyes and mouth, issues with viscera — especially with the digestive tract, heart, lungs, and kidneys — skin sensitivity to sunlight, weight loss, and a great host of others. These typically make themselves felt in occasional ‘flares’, and then (especially with treatment) go into remission, when the symptoms can be abated completely.
Now, because of the wide range of symptoms it can produce, SLE is extremely hard to diagnose directly, as it fits the description of a large number of other diseases. It’s one of the conditions known as ‘great imitators’ because of this, and an SLE diagnosis is almost always placed by ruling out other diseases. This usually involves a pretty long process of consultations and lab analyses, including bloodwork.
Ok, so what causes it?
Like all autoimmune diseases, the problems are caused by our own immune system. It’s either too passive, giving pathogens an easy in, or too active, which makes it attack our own tissues (as in the case of lupus).
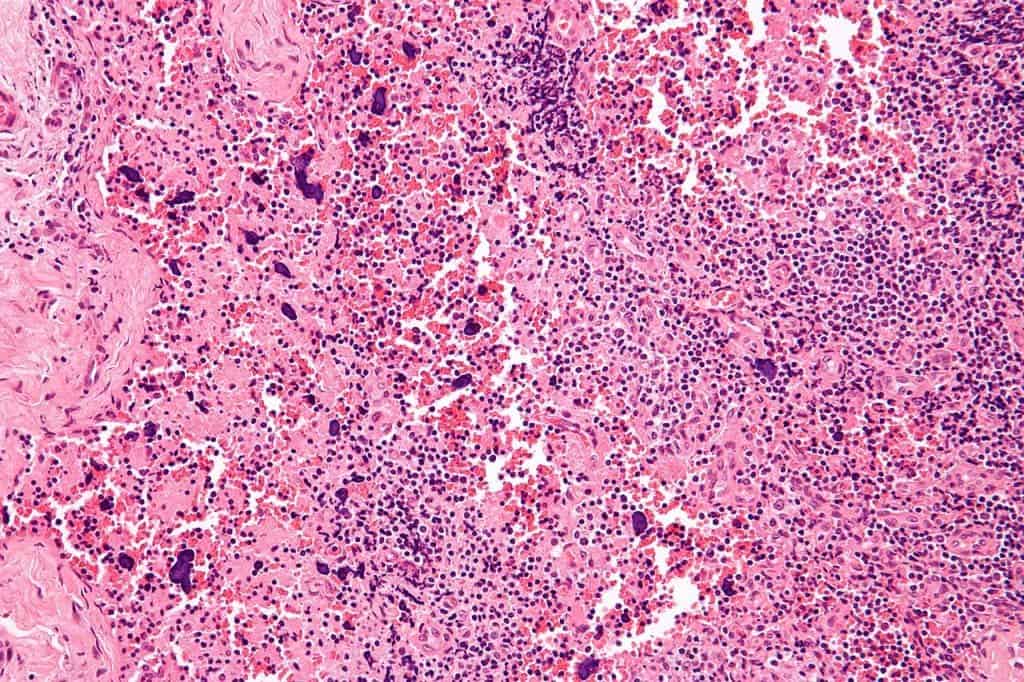
While we do know that this is mediated by autoantibodies, we don’t know for sure what causes SLE in the first place. We’re pretty confident that genetic factors have a role to play, as women represent the majority (around 90%) of cases; people with a history of lupus in their family are also more at risk of developing the condition themselves, although they don’t necessarily have to. Even among identical twins, if one develops lupus there is only a roughly 1-in-4 chance for the other to develop it as well. While we’re certain that there is a genetic component to lupus, we’ve yet to identify a single gene that’s responsible for its onset.
Environmental factors, however, also seem to matter. “Hormonal, as well as immune abnormalities” also play a part, according to “Lupus: An Overview of the Disease And Management Options” (Maidhof, Hilas, 2012). The most glaring example here would be drug-induced lupus erythematosus, whose onset is associated with long-term drug treatments and represents 6% to 12% of all lupus cases. “Hundreds of drugs have been reported to cause” the condition, the study adds. Its symptoms are very similar to those of SLE but reversible, and generally go away after the treatment is interrupted or runs its course.
While its cause is still unclear, we do have a good understanding of how SLE functions on a cellular level.
“The antigens in patients with SLE can be attributed to the inappropriate disposal of apoptotic [dying] cells,” the authors explain. “During the process of cellular death, pieces of cellular material form on the surface of the dying cell. Antigens that are normally absent on the surface of the cellular material, but instead are embedded within, are now present on the cell surface.”
“It is believed that the removal of these apoptotic cells is compromised because of the impaired functioning of phagocytic cells, resulting in suboptimal disposal of dying cells and antigen recognition in patients with SLE.”
Treatment, management
The short of it is that we don’t have any cure for SLE. It is a chronic condition that affects patients for life. We can manage the symptoms with treatment and limit the condition’s effect on the body to an extent, but we don’t have anything that will make the actual disease go away yet.
So what is our treatment strategy, then? Well, the most important parts of it are to prevent flare-ups, limit or neutralize the symptoms during flare-ups, and prevent (though more usually, to limit) the amount of damage SLE causes to a patient’s internal organs. The most common way to do this is through the administration of drugs that dampen the function of a patient’s immune system.
One of the most commonly-prescribed treatment courses against SLE are anti-inflammatory drugs, both of the corticosteroid and non-steroid varieties. Nonsteroidal drugs (think Ibuprofen) are typically less effective at controlling pain and inflammation than corticosteroids so they can’t really manage the symptoms of most patients. Corticosteroids are much more powerful, and in high doses can calm down the activity of the immune system quite significantly. However, they’re trickier to use right. Stopping the treatment suddenly can and will harm the patient’s body, so corticosteroids are prescribed with a lower and lower dosage as the treatment progresses. While they’re very effective at treating the symptoms of SLE, the longer they’re used, the harder and more dangerous it is to wean a patient off the compounds.
Antimalarial drugs are also, surprisingly, a good treatment option for SLE. They address many of the same symptoms — swollen, painful joints, skin rashes, lung inflammation, and fatigue. Despite being designed against malaria, they’re generally quite effective at managing SLE symptoms and preventing flare-ups.
The most severe cases generally receive treatment with dedicated immunosuppressives, even chemotherapy. Because they pose a whole lot of risks for patients, however, these are only employed for cases where major organs are affected and other treatment options don’t seem to work.
Not to be the bearer of bad news or anything but Lupus doesn’t have a very good long-term prognosis. Not the condition itself, to be precise, but the complications that flow from it. Issues with internal organs, most commonly the heart or kidneys, are leading causes of death for SLE patients, as are infections. Still, we’ve made great strides in understanding lupus and how to manage its symptoms.
Back two decades ago, the 5-year survival rate for patients in Toronto was 92% according to (Gordon, 2002) “Long‐term complications of systemic lupus erythematosus”, falling to 82% at 10 years, 76% at 15 years, and 68% at 20 years, although this is significantly higher than the rates seen in around the 1950 period, mostly due to better treatments and faster diagnostics. Still, these figures assume that the patients are getting quality healthcare quite rapidly, as the figures are reported for patients in a wealthy, industrialized country. These survival figures have been inching up over the years, and are likely still doing so.
Also, keep in mind that “82% survival at 10 years” doesn’t mean “18% of patients died 10 years after the diagnosis”. It is meant to show how many years the participants were involved in the study, with them being enrolled after diagnosis, and the survival rate by that point. So 82% of the participants were still alive after a 10-year monitoring period, but the researchers didn’t follow up on them after this point (i.e. we don’t know how old they were when they died). Individual participant age is also a factor that can influence the overall survival rate seen in these studies.
Even so, lupus patients “still have a mortality risk equal to three times that of the general population […] despite the improvement in survival rate”. The way we treat its symptoms is, arguably, contributing to this increased mortality risk — our immune system, after all, is meant to keep us alive. But we do have ways to work around that, and most SLE patients today (between 80% to 90%, typically those with mild or moderate cases) can expect to live a full life.